 |
 |
- Search
| J Acute Care Surg > Volume 12(1); 2022 > Article |
|
Abstract
Purpose
Traumatic duodenal injury is uncommon and due to its difficult diagnosis and accessibility there is an increased risk of mortality and morbidity.
Methods
Electronic medical records of a single center were reviewed retrospectively from March 2008 to December 2020 and a total of 7 cases of traumatic duodenal injury were managed by surgical exploration. The site of duodenal perforation, injury mechanisms, operation method, and postoperative outcomes were assessed.
Results
The mean age was 55.72 years (range, 34ŌĆō78), and there were 5 men in the study. The most common mechanism was in-car traffic accident (4 cases), and 1 case each of pedestrian accident, accident during work, and self-injured stab wound. The most common site of injury was between the 3rd and 4th portion (3 cases), followed by the bulb and 1st portion (2 cases), and 2nd portion (2 cases). Segmental resection of the duodenum and primary anastomosis was performed in the 3rd and 4th portion perforation. In cases of 1st and 2nd portion, injury was managed by primary repair or pylorus preserving pancreaticoduodenectomy. Complications developed in 4 patients, and the most common complication was a problem with the wound; wound seromas developed in 4 cases, entero-cutaneous fistula in 1, and biliary complications in 2 cases. Two patients suffered from intraperitoneal abscess or fluid collection managed by percutaneous drainage. The mean duration of hospital stay was 34 days, and postoperative mortality did not develop.
Traumatic duodenal injury is regarded as a ŌĆ£real challengeŌĆØ for trauma surgeons. The incidence of duodenal injury from trauma forms a relatively small portion, less than 5% of all abdominal injuries [1ŌĆō3]. However, due to its diversity of location and the extent of injury in each patient, traumatic duodenal injury has shown a wide range of associated morbidity and mortality from 5% to 55% [4,5].
The current consensus suggests therapeutic plans for traumatic duodenal injuries should be based on the American Association for the Surgery of Trauma organ injury scale, which has 5 classes of severity [6]. In clinical practice, optimal management varies with the mechanism of trauma, location, and degree of injury (including the associated organ or major vessel injuries) [7]. Moreover, it is difficult for clinicians to detect duodenal injury in the early phase of trauma due to the presence of retroperitoneal space, which results in delayed diagnosis with development of sepsis [8]. In this study, 7 cases of traumatic duodenal injuries managed by surgical approaches were reviewed.
Electronic medical records of a single center in Korea were retrospectively reviewed from March 2008 to December 2020. The patients selected for this study were traumatized patients who were older than 20 years, and injured by a blunt or penetrating mechanism. Postprocedural injuries including esophago-gastroduodenoscopy, endoscopic retrograde cholangiopancreatography, radiographical interventional procedures, or postoperative duodenal perforations were excluded. Patient data including location, and mechanism of injury, the type of surgical management, and postoperative clinical outcomes were collected.
Perforation of the duodenum was diagnosed using an abdominopelvic computed tomogram (CT) scan or was based on intraoperative findings. Duodenal perforation was suspected: (1) when the free air in the retroperitoneal or the space around the duodenum with the hematoma formation was around the superior mesenteric root; (2) or when there were mucosal defects, or tearing, or abnormal thickening of the duodenum; and (3) when there was free air in the peritoneal space along the duodenal bulb or ampulla (Figure 1). The method of surgery was decided based on the injury site or surgeonsŌĆÖ preference. The method for segmental resection of duodenum 3rd and 4th portions, and duodenojejunostomy was added (Figure 2). This study was approved by Severance Hospital Institutional Review Board (no.: 4-2021-0959), and informed consent was waived due to the retrospective nature of the study.
A total of 7 cases with traumatic duodenal injury were managed by surgical exploration at a single institution over a 12-year period. The mean age was 55.7 years, and the most common mechanism of trauma was an in-car traffic accident. The most common site of duodenal injury was between the 3rd and 4th portion (3 cases) followed by the bulb, 1st portion (2 cases), and 2nd portion (2 cases). Segmental resection of the duodenum and duodenoduodenostomy or duodenojejunostomy was performed in the 3rd and 4th portions to repair perforations. In cases of the 1st and 2nd portions, injury was managed by primary repair or pylorus preserving pancreaticoduodenectomy (PD). The details of each patient are described in Table 1.
Postoperative clinical outcomes during hospital stays are shown in Table 2. Four patients had postoperative complications, and 3 patients needed re-operation or percutaneous interventions to treat their complications. The mean length of hospital stay was 34 days, and there was no event of death in this study.
The operative decision for traumatic duodenal injuries is usually difficult for clinicians due to the possibility of delayed diagnosis and associated injuries of adjacent organs or vessels [7]. Patients with retroperitoneal organ injuries often exhibit vague symptoms in the early stage of injury. Therefore, when serious symptoms develop, the patients are likely in septic shock or ongoing multiorgan failure resulting in mortality.
The current clinical practice in the treatment of traumatic duodenal injuries varies based on the surgeonŌĆÖs experience. However, a common trend is a shift from complex operative techniques to simpler procedures. Aiolfi et al [9] demonstrated an increased likelihood of undergoing less invasive procedures for traumatic duodenal injuries during the period 2007ŌĆō2014 compared with 2002ŌĆō2006. In addition, they reported significantly improved mortality in patients from the 2007ŌĆō2014 period, and concluded that the use of less invasive procedures may lead to better survival outcome.
A recent retrospective review of 15 patients managed with damage control surgery and staged Whipple operation, or with conventional Whipple operation as their 1st operation, also demonstrated the benefits of damage control surgery in patients with the lethal triad including acidosis, hypothermia, and coagulopathy [10]. They reported an in-hospital mortality rate of 13%, which was less than half of the recent series [10]. In this current study, all 7 patients arrived hemodynamically stable with a systolic blood pressure of more than 90mmHg, and had no need for transfusion because their initial level of hemoglobin was over 10.0 mg/dL before the operation. Therefore, the 1-stage operation of bowel resection with primary reconstruction could be performed in all cases without mortality.
Although less invasive procedures for traumatic duodenal injuries have been suggested for the last decade, studies [2,11] have shown no increased risk of mortality in selected patients with penetrating duodenal injury managed by PD compared with those who underwent laparotomy without PD. Grigo et al [11] reported that modern traumatic PD showed improved mortality in line with elective PD performed in cancer patients. The key components of these improved clinical outcomes include an improvement in postoperative management with notable advances in radiological interventions, endoscopic approaches, standardized protocols, and critical care [12ŌĆō14]. The considerable progress in dealing with postoperative complications has led to reduced morbidity and mortality after PD, and this observation is also applicable to traumatic PD.
In this current study, there were 7 cases of duodenal injury from various mechanisms of trauma. Two experienced trauma surgeons made surgical decisions based on the severity of injury and patientsŌĆÖ status after resuscitation. All the patients in this study also underwent surgical interventions within 24 hours of injury. Unlike the current trend, a major resection of the duodenum was performed in 3 patients, pyloric exclusion in 1 patient, and PD in 2 patients. Only 1 case of penetrating injury underwent primary repair of the duodenum. Over the 12-year study period, there was no mortality among patients who underwent major resections.
This study has several limitations. Firstly, due to the lack of traumatic duodenal perforation, the number of cases was small. Therefore, statistical analysis could not be performed. Secondly, the collected data were extracted from a single center. In Korea, regional trauma centers were established in 2014, however, this data was not collected. Despite these limitations, this study may be helpful when deciding on the surgical management for perforation of the duodenum.
We reported favorable clinical outcomes in patients with traumatic duodenal injury managed by various surgical approaches. There is a call for flexible applications of diverse surgical options according to the patientsŌĆÖ condition, and the severity of injury and accessible facilities in each institution.
Acknowledgments
This manuscript was presented at the 8th International Congress of World Society of Emergency Surgery.
Notes
Figure┬Ā1
Suspected duodenal perforation visualized using an abdominopelvic computed tomogram scan. (A) Retroperitoneal free air was noted over the duodenum along the pancreas. (B) Hematoma around the superior mesenteric root was noted.

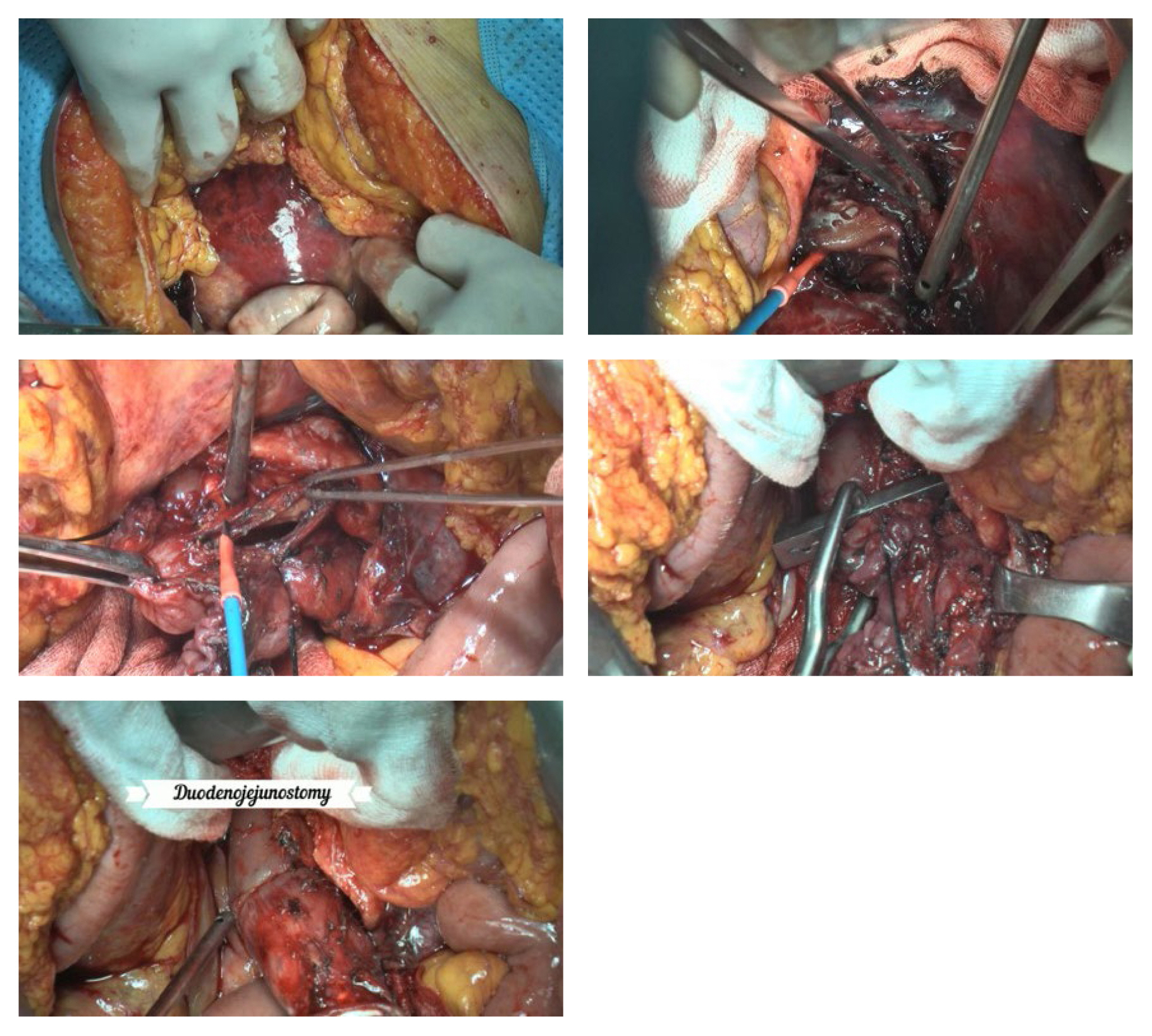
Figure┬Ā2
Surgical technique. Hematoma and bulging of retroperitoneal space under the transverse mesocolon. After the opening of the mesocolon a torn duodenum was detected. The duodenal 4th portion was nearly all transected (90%, 4 cm in length). After the TreitzŌĆÖs ligament was opened, the retroperitoneal duodenum was mobilized from the surrounding tissue. The 3rd portion of duodenum was also mobilized after Kocherization. Then, the duodenum was resected proximally at the distal 2nd portion, and the proximal jejunum was resected distally just below the TreitzŌĆÖs ligament. After the anvil was inserted, the duodenojejunostomy using a gastrointestinal anastomosis stapler was conducted with a direct view of the ampulla of Vater to avoid injury of the ampulla.
Table┬Ā1
Comparison of patients based on presence or absence of HVI.
| Pt. | Mechanism | Sex/age (y) | Location | Severity of injury* | Associated abdominal organ injury | Initial hemodynamicsŌĆĀ | Total amounts of pre/intra-operative transfusion (PRBCs, units) | Types of operation |
|---|---|---|---|---|---|---|---|---|
| 1 | Blunt (in-car TA) | M/34 | 2ndŌĆō3rd | 3 | Stomach | 123/86 mmHg 104/min, 36.1┬░CŌĆĀ | 0/1 | Segmental resection of duodenum with duodenoduodenostomy Wedge resection of stomach |
| 2 | Blunt (in-car TA) | M/34 | 2nd | 3 | Transverse colon Liver | 99/62 mmHg 108/min, 36.7┬░CŌĆĀ | 0/0 | Pyloric exclusion with gastrojejunostomy Segmental resection of transverse colon with end- to-end anastomosis Diverting loop ileostomy Bleeder ligation of liver |
| 3 | Penetrating (stab) | F/38 | Duodenal bulb | 2 | None | 98/59 mmHg 60/min, 36.5┬░CŌĆĀ | 0/0 | Primary repair of duodenum |
| 4 | Blunt (out-car TA) | F/67 | 3rd | 3 | None | 112/73 mmHg 80/min, 35.8┬░CŌĆĀ | 0/3 | Segmental resection of duodenum with duodeno- duodenostomy |
| 5 | Blunt (fall) | M/62 | Duodenal bulb | 5 | Pancreas head Stomach | 115/82 mmHg 130/min, 36.6┬░CŌĆĀ | 0/0 | Conventional pancreaticoduodenectomy |
| 6 | Blunt (motorcycle) | M/77 | 2nd (posterior) | 4 | None | 140/96 mmHg 126/min, 36.8┬░CŌĆĀ | 0/0 | Pylorus-preserving pancreaticoduodenectomy |
| 7 | Blunt (in-car TA) | M/78 | 3rd | 3 | Terminal ileum | 105/70 mmHg 86/min, 35.9┬░CŌĆĀ | 0/1 | Segmental resection of duodenum with duodeno- jejunostomy Segmental resection of small bowel with end-to-end anastomosis |
Table┬Ā2
Clinical outcome during hospital stay.
References
1. Asensio JA, Feliciano DV, Britt LD, Kerstein MD. Management of duodenal injuries. Curr Probl Surg 1993;30(11):1026ŌĆō92.

2. Krige JE, Nicol AJ, Navsaria PH. Emergency pancreatoduodenectomy for complex injuries of the pancreas and duodenum. HPB(Oxford) 2014;16(11):1043ŌĆō9.



3. Antonacci N, Di Saverio S, Ciaroni V, Biscardi A, Giugni A, Cancellieri F, et al. Prognosis and treatment of pancreaticoduodenal traumatic injuries: Which factors are predictors of outcome? J Hepatobiliary Pancreat Sci 2011;18(2):195ŌĆō201.


4. Blocksom JM, Tyburski JG, Sohn RL, Williams M. Prognostic determinants in duodenal injuries. Am Surg 2004;70(3):248ŌĆō55.



5. Ballard RB, Badellino MM, Eynon CA, Spott MA, Staz CF, Buckman RF. Blunt duodenal rupture: A 6-year statewide experience. J Trauma Acute Care Surg 1997;43(2):229ŌĆō33. discussion 233.

6. Moore E, Cogbill T, Malangoni M, Jurkovich G, Champion H, Gennarelli T, et al. Organ injury scaling, II: Pancreas, duodenum, small bowel, colon, and rectum. J Trauma 1990;30(11):1427ŌĆō9.


7. Lucas CE. The therapeutic challenges in treating duodenal injury. Panam J Trauma Crit Care Emerg Surg 2013;2(3):126ŌĆō33.

8. Crippa S, Falconi M, Bettini R, Barugola G, Germenia S, Salvia R, et al. Isolated blunt duodenal trauma: Delayed diagnosis and favorable outcome with ŌĆ£quadruple tubeŌĆØ decompression. JOP 2007;8(5):617ŌĆō20.

9. Aiolfi A, Matsushima K, Chang G, Bardes J, Strumwasser A, Lam L, et al. Surgical trends in the management of duodenal injury. J Gastrointest Surg 2019;23(2):264ŌĆō9.



10. Thompson CM, Shalhub S, DeBoard ZM, Maier RV. Revisiting the pancreaticoduodenectomy for trauma: A single institutionŌĆÖs experience. J Trauma Acute Care Surg 2013;75(2):225ŌĆō8.



11. Grigorian A, Dosch A, Delaplain P, Imagawa D, Jutric Z, Wolf R, et al. The modern trauma pancreaticoduodenectomy for penetrating trauma: A propensity-matched analysis. Updates Surg 2021;73(2):711ŌĆō8.



12. Cusworth BM, Krasnick BA, Nywening TM, Woolsey CA, Fields RC, Doyle MM, et al. Whipple-specific complications result in prolonged length of stay not accounted for in ACS-NSQIP Surgical Risk Calculator. HPB(Oxford) 2017;19(2):147ŌĆō53.









