|
 |
- Search
| J Acute Care Surg > Volume 12(3); 2022 > Article |
|
Abstract
Purpose
In the Republic of Korea, the use of trauma centers was recently adopted and is expected to have better outcome for severely injured patients. This study aimed to evaluate the clinical outcomes and treatment methods for unstable pelvic bone fractures in trauma centers.
Methods
The annual number of patients, clinical outcomes, and treatment methods of unstable pelvic bone fractures in three trauma centers from 2016 to 2020 were retrospectively reviewed. The patients were dichotomized into survivors and deceased, and demographic data, treatment, and clinical outcomes were compared. Multivariable analysis was performed to identify the factors associated with survival.
Results
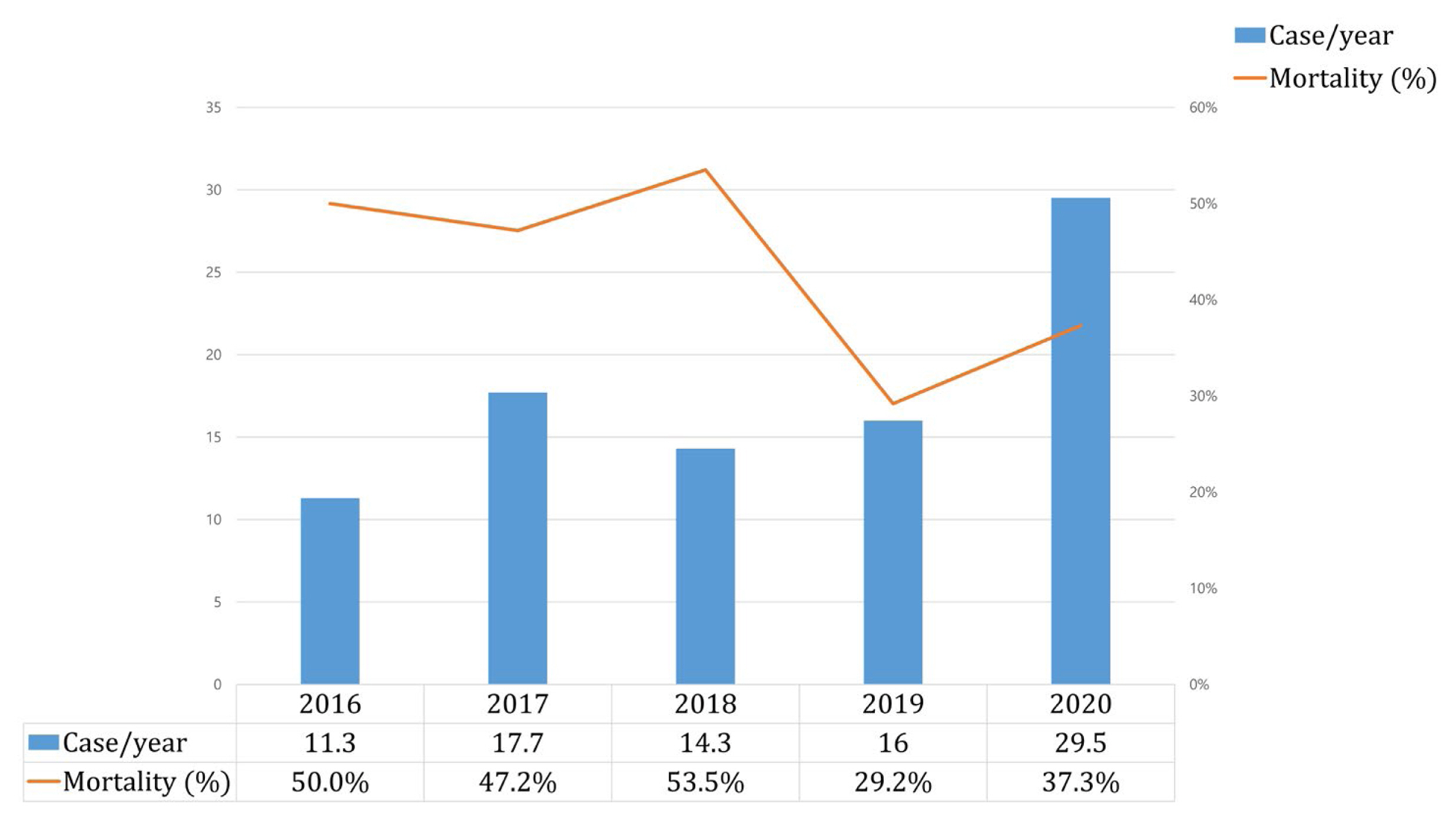
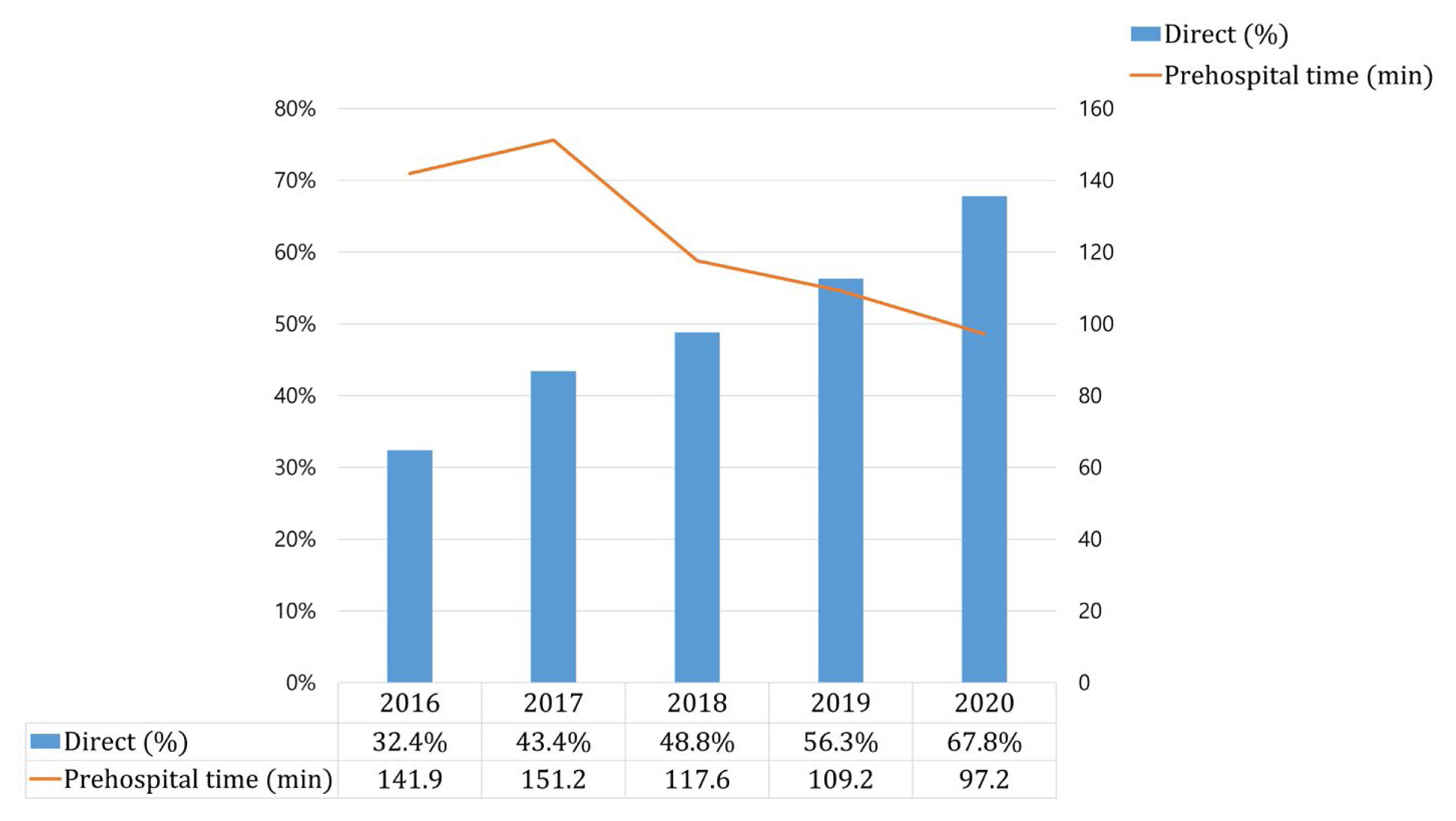
Among 237 patients, 101 (42.6%) were deceased. Mortality was lower in the later period (2019–2020) compared with the early period (2016–2018; 33.6% vs. 50.0%, p = 0.011). Direct admission of an increasing number of patients to trauma centers reduced prehospital time. Although the use of angioembolization in treating pelvic bone fracture (p < 0.001), and the use of other treatment methods did not change significantly (2016–2020). Lower age, lowest systolic blood pressure in the trauma bay, and higher lactate level, international normalized ratio, the amount of packed red blood cell transfusion at 24 hours were positively associated with mortality in the multivariate analysis.
Severe pelvic bone fracture is associated with a high mortality rate. Although various treatment methods, including preperitoneal pelvic packing (PPP), angioembolization, temporary pelvic fixation, and resuscitative endovascular balloon occlusion of the aorta (REBOA), have been studied for the management of these fractures; the optimal treatment method is still unclear [1]. In addition to these treatment methods, systematic approaches to facilitate rapid response and multidisciplinary treatment are also important in the management of pelvic bone injury. Therefore, the government of the Republic of Korea founded a national trauma system and built regional trauma centers, which have reduced preventable death rates among trauma patients [2]. Since then, many domestic studies on severe pelvic bone fractures have been conducted, but most were single-center studies because each trauma center would assess its own protocol [3–7].
Trauma centers in the Republic of Korea are expected to report their data to the Korean Trauma Data Bank (KTDB), similar to the National Trauma Data Bank in the US. However, the KTBD is not an open source, nor is it utilized or shared liberally. In addition, specific data related to pelvic injury treatment such as the use of angioembolization and PPP, has not been included in the KTDB, making it difficult to study cases of severe pelvic bone fracture. However, multi-institutional studies are essential due to the low incidence and high mortality of these fractures. In addition, treatment guidelines or protocols should be based on multi-center databases.
Thus, the objectives of this study were to investigate the clinical outcomes of pelvic bone fracture based on trauma center data to identify feasible treatment methods, and review KTDB data to create a pelvic bone fracture-specific database.
Data from medical records of three regional trauma centers was collated in this retrospective study which was approved by the institutional review board at each hospital (no.: AJIRB-MED-MDB-22-167 / DKUH 2022-06-041 / CR-322088). The participating centers were tertiary university hospitals that had been designated as regional trauma centers before 2016. Inclusion and exclusion criteria were based on the KTDB. Cases of severe pelvic bone fracture [abbreviated injury scale (AIS) 4 with either initial systolic blood pressure ≤ 90 mmHg or massive transfusion of ≥ 10 units of packed red blood cells within 24 hours] from January 2016 to December 2020 were included in the study. Exclusion criteria were age under 18 years and open fracture (AIS codes 856162.4 and 856174.5).
The KTDB includes prehospital and hospital clinical data but does not contain information regarding treatment methods. Thus, treatment method and laboratory data were collected separately. The treatment method included PPP, angioembolization, REBOA, laparotomy, pelvic binder, or external fixation. However, the data for pelvic binder and external fixation contained many missing values and a small number of cases, therefore, analyses of these methods could not be performed. Angioembolization included selective and nonselective embolization, and was performed at the discretion of the interventionists. Annual changes in patient number, clinical outcomes, and treatment methods were reviewed. A linear-by-linear association test was used to assess changes in treatment methods. Patient data was dichotomized into survivor and deceased patient groups, and the demographic and clinical data of the two groups were compared.
After assessing the data for normality using the Kolmogorov–Smirnov test, continuous variables were compared between the groups using the Mann–Whitney U test, and the data were presented as median values (interquartile range). Categorical variables were compared between the groups using the chi-square test or Fisher’s exact test. Binary logistic regression was applied to identify factors associated with survival and included treatment methods. All analyses were performed using SPSS Version 23.0 (IBM Corp., Armonk, NY, USA).
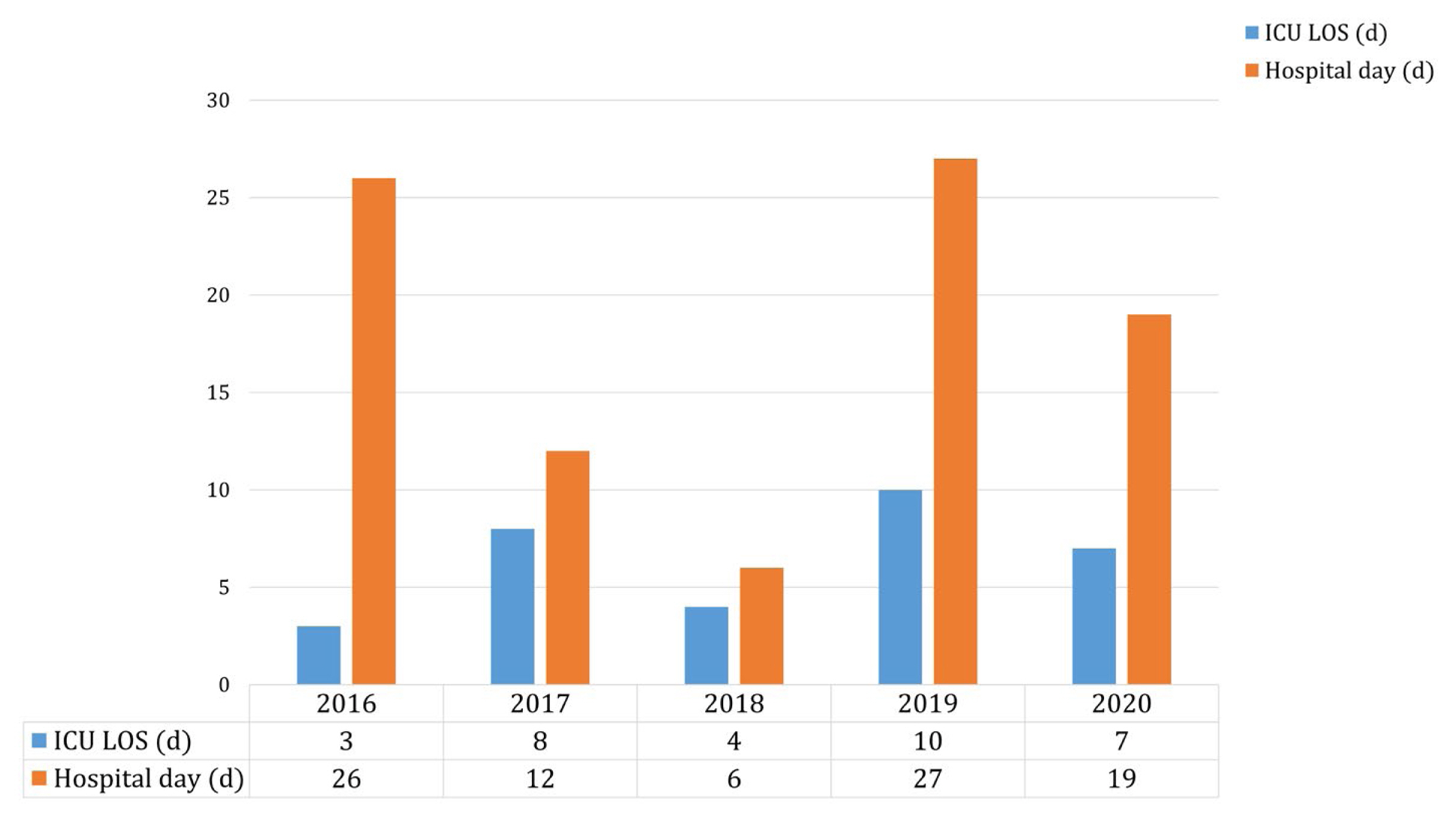
In this retrospective study of clinical outcomes, and treatment methods of unstable pelvic bone fractures from 2016–2020, a total of 237 patients were included, of which 136 (57.4%) patients survived. Although the number of patients admitted to each trauma center was similar across years, it almost doubled in 2020. Mortality was lower in the later period (2019–2020) than the early period (2016–2018; 33.6% vs. 50.0%, p = 0.011; Figure 1). The median injury severity score increased year on year (Table 1). Mortality was the highest in 2018, while the duration of hospitalization was the shortest in this year. (Figure 2). A gradually increasing number of patients were directly admitted to the trauma centers, thereby resulting in a reduction in prehospital time (Figure 3).
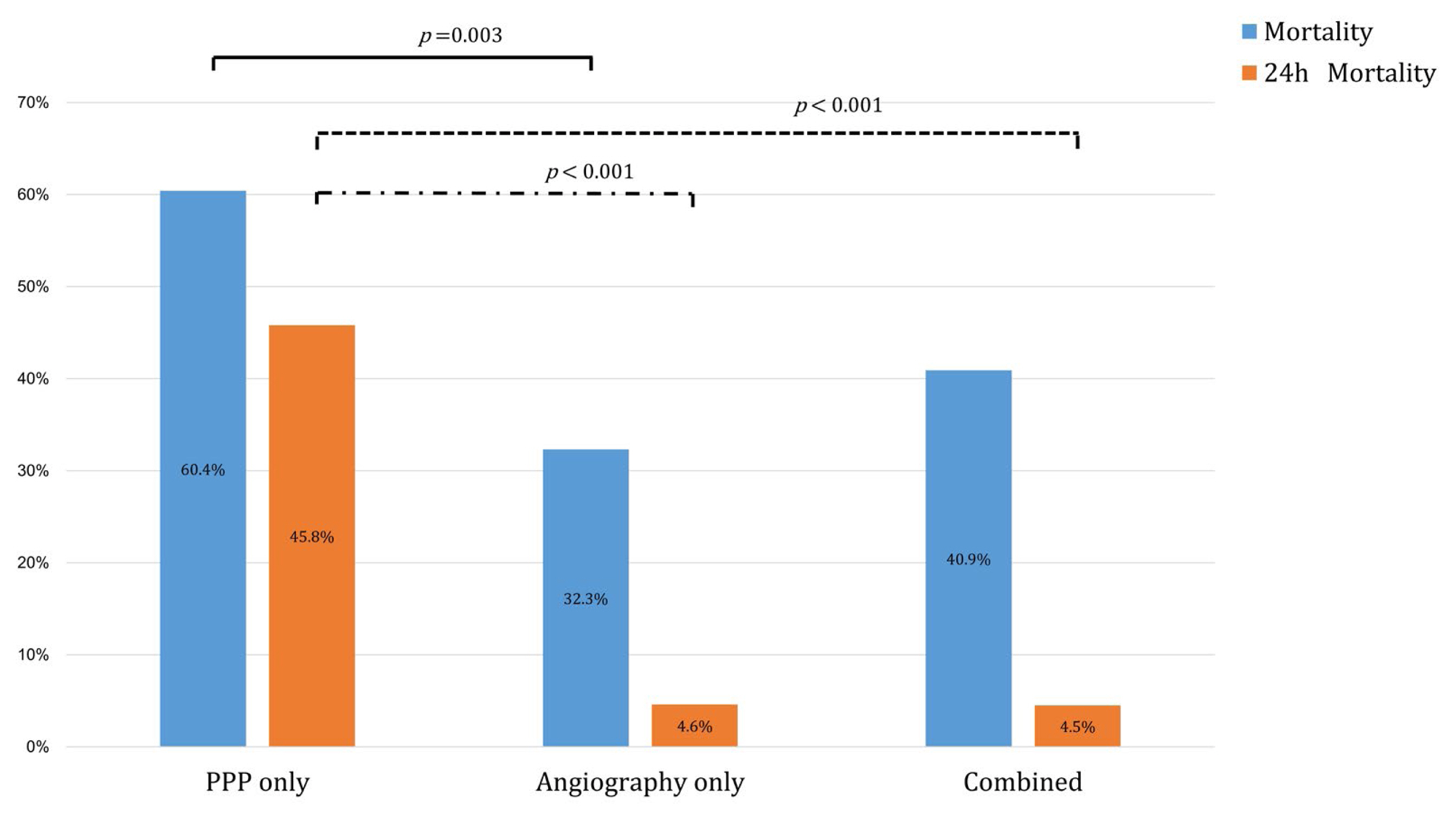
Among the patients receiving different treatments, the PPP-only group showed significantly higher overall mortality and 24-hour mortality compared with the angiography-only, and combined angioembolization and PPP groups (Figure 4). The utilization of angioembolization showed an increasing trend over the study period (p < 0.001), but PPP utilization did not significantly change (p = 0.535) over the study period. The utilization of combined angioembolization and PPP also increased over the study period (p < 0.001). REBOA was the most frequently utilized method in 2018, but mortality was also the highest in the same year (Figure 5).
Surviving patients showed significantly better initial vital signs and laboratory data and required less packed red blood cell transfusion. The usage rate of PPP was significantly higher in the deceased group (46.5% vs. 33.1%, p = 0.036), and angioembolization was higher in the survivor group, albeit without statistical significance (51.5% vs. 39.0%, p = 0.058). REBOA utilization was higher in the deceased group (34.7% vs. 11.0%, p < 0.001; Table 2). In the multivariate analysis, higher age, lactate level, international normalized ratio, amount of packed red blood cell transfusion within 24 hours and lower the lowest systolic blood pressure were associated with mortality. However, the treatment method was not associated with mortality (Table 3).
An increasing trend of centralization to trauma centers, with an elevated number of patients being directly admitted to the trauma centers in 2020 was observed in this study. This trend also resulted in a gradual reduction in the annual prehospital time. The government in the Republic of Korea developed a trauma care system to decrease the death rates attributable to preventable trauma. There were eight regional trauma centers officially opened in December 2015. Moreover, the 119 national emergency system included a new transport guideline mandating the transportation of patients with severe trauma to be taken to regional trauma centers instead of the nearby hospital. Jung et al [2] reported that trauma centers had lower preventable trauma death rates than non-trauma centers, and that transfer was a risk factor for preventable trauma-related death. The importance of directly transferring severe trauma patients to a trauma center within the appropriate time was highlighted [2]. In the current study, shortening the prehospital time was observed to improve clinical outcome. Although the number of patients with unstable pelvic bone fractures did not increase between 2016 and 2019, the proportion of direct admissions to trauma centers showed a continued increase.
The development of trauma centers has resulted in the improvement in mortality rates associated with severe pelvic bone injury in the Republic of Korea [3]. Jang et al [8] reported that the improvement was attributable to an increased use of emergency procedures such as PPP and angiography. However, unlike angiography, the use of PPP did not increase over the years despite an improvement in mortality rates in the recent period. As a result, angiography seemed to be associated with survival, while PPP was associated with death in the univariate analysis. In the multivariate analysis, PPP also showed a favorable tendency for survival (odds ratio: 1.816; p = 0.147), similar to angiography (odds ratio: 1.661; p = 0.179). However, neither treatment showed statistical significance. PPP is a key procedure in the treatment of unstable pelvic bone injury [1]. Unlike other procedures, PPP can be immediately performed at the bedside, making it an effective damage control technique for sole bleeding control or in conjunction with either angioembolization or external fixation [9]. In a quasi-randomized trial, PPP was reported to have a much shorter time to intervention compared with angioembolization, and had similar mortality [10]. In addition, the main source of bleeding in cases with hemodynamically unstable pelvic ring disruptions was venous bleeding [1]. Therefore, PPP could be utilized for the initial treatment of hemodynamically unstable pelvic bone injury. Additional treatments such as angiography or laparotomy, could be applied if continuous bleeding is suspected. Moreover, many studies have evaluated the effectiveness of PPP, and it has been recommended for the initial management of unstable pelvic fractures [11–13]. In this study, PPP was associated with death in univariate analysis. However, PPP appears to have been used for hemodynamically unstable patients who required immediate additional treatment. We do not believe that PPP is a harmful procedure for pelvic injury management.
Angioembolization is another important treatment method. Salcedo et al [14] demonstrated that pelvic angioembolization is the most effective intervention for the management of hemorrhage in both hemodynamically stable, and unstable patients. Li et al [10] reported a randomized trial comparing PPP and angioembolization, and observed similar outcomes. However, angiography plays a limited role since it can only treat arterial bleeding, and it requires time for preparation. In the current study, the time to angiography was approximately two hours after admission, which may be too late for bleeding control. In addition, although treatment with only angiography yielded more favorable outcomes compared with only PPP, these patients appeared to present with relatively stable vital signs after resuscitation. Since the time from admission to angiography was approximately double that for PPP, these patients may have undergone maintenance of vital signs during the preparation of angioembolization. In addition, treatment methods were not associated with survival in multivariate analysis.
Nevertheless, the 24-hour mortality in the combined PPP and angioembolization group was significantly lower compared with the PPP-only group although severity was not adjusted. Therefore, angioembolization could be considered after PPP. Similarly, PPP could be utilized in conjunction with angioembolization or temporary external fixation, and be performed as a bedside procedure. A combination of PPP and angiography has been recommended for the treatment of hemodynamically unstable pelvic bone fractures in recent guidelines [1,15].
REBOA is an increasingly prominent treatment method for severe pelvic bone injury. In a review in 2016, soon after the implementation of trauma centers, the clinical outcomes of REBOA were not favorable because the technique was applied in desperate cases [16]. However, recently, the effectiveness of this technique, in combination with detailed indications and a better resuscitation strategy, has been reported [17,18]. In addition, the technique has been reported to prevent cardiac arrest and could be utilized for bridging procedures in cases requiring definite hemostatic treatment [19]. REBOA was only recently adopted in the Republic of Korea, and experience in technique is therefore limited [20,21]. In our study, REBOA was the most frequently used technique in 2018, but mortality was the highest in that year; it was not used as frequently in 2019–2020 compared with 2018. However, this finding does not preclude the use of REBOA, it can be a powerful resuscitation tool. Evidence of its effectiveness needs to be studied in more detail.
Age, lactate level, international normalized ratio, amount of packed red blood cell transfusion within 24 hours, and lowest systolic blood pressure were associated with mortality in this study. Except for age, the other factors might be modifiable and are related to massive bleeding, and coagulopathy [22]. This indicates the need for a strategy for early correction of coagulopathy and definite control of hemorrhage. The strategy requires a multidisciplinary approach since no single treatment method has been reported to yield superior findings [1].
This study had several limitations. Firstly, although this was a multi-institutional study involving three hospitals, other trauma centers exist in the Republic of Korea, and patients’ centralization to these trauma centers might be different. However, the three trauma centers in this study were designated in the early period of setting up trauma centers and these centers reported on pelvic fracture [3,4,7,8,20]. Secondly, data for pelvic fixation procedures, such as pelvic binders or external fixation data, were not included. The KTDB does not have such data, and there is no treatment code for pelvic binders. Thus, the use of pelvic binders could be inferred only from nurses’ or doctors’ records, and there were many missing values as a result. Therefore, a detailed analysis could not be performed, and a pelvic bone-specific database set that included these data should be developed for further studies. Thirdly, many poly-trauma patients who may have also had severe injuries other than pelvic injuries were included. Fourthly, the number of patients increased in 2020 during the height of the coronavirus disease-19 pandemic when more patients attended trauma centers [23].
In conclusion, a gradually increasing number of patients with hemodynamically unstable pelvic bone fractures were directly admitted to the trauma center, and the mortality rate associated with these fractures also improved. Among the treatment modalities for these patients, angioembolization, and PPP showed a continuous increase in use. Although the treatment method was not associated with survival in multivariate analysis, angiography might be considered if PPP was performed. Since coagulopathy-related factors were associated with survival, a treatment strategy for early bleeding control is essential.
Notes
Figure 5
Annual changes in treatment methods.
PPP = preperitoneal pelvic packing; REBOA = resuscitative endovascular balloon occlusion of the aorta.

Table 1
Patients’ demography and injury severity between 2016 and 2020.
| 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|
| Age (y) | 53 (45–71) | 59 (47–73) | 59 (45–73) | 59 (51–66) | 58 (35–70) |
|
|
|||||
| Sex, male (%) | 52.90 | 69.80 | 69.80 | 58.30 | 67.80% |
|
|
|||||
| ISS | 32 (29–43) | 36 (29–43) | 38 (27–43) | 40 (29–44) | 43 (38–51) |
|
|
|||||
| TRISS* | 0.88 (0.37–0.93) | 0.62 (0.46–0.85) | 0.83 (0.60–0.91) | 0.68 (0.55–0.82) | 0.7 (0.39–0.87) |
|
|
|||||
| Abbreviated Injury Scale | |||||
| Head ≥ 3 (%) | 23.50 | 24.50 | 18.60 | 25.00 | 30.50% |
| Thorax ≥ 3 (%) | 47.10 | 50.90 | 58.10 | 77.10 | 71.20% |
| Abdomen ≥ 3 (%) | 52.90 | 45.30 | 51.20 | 62.50 | 42.40% |
Table 2
Patient and injury characteristics.
Table 3
Univariate and multivariate analysis for survival.
References
1. Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg 2017;12:5.




2. Jung K, Kim I, Park SK, Cho H, Park CY, Yun JH, et al. Preventable trauma death rate after establishing a national trauma system in Korea. J Korean Med Sci 2019;34(8):e65.




3. Jang JY, Bae KS, Chang SW, Jung K, Kim DH, Kang BH. Current management and clinical outcomes for patients with haemorrhagic shock due to pelvic fracture in Korean regional trauma centres: A multi-institutional trial. Injury 2022;53(2):488–95.


4. Jang JY, Shim H, Jung PY, Kim S, Bae KS. Preperitoneal pelvic packing in patients with hemodynamic instability due to severe pelvic fracture: Early experience in a Korean trauma center. Scand J Trauma Resusc Emerg Med 2016;24:3.



5. Kim H, Jeon CH, Kim JH, Sun HW, Ryu D, Lee KH, et al. Transarterial embolisation is associated with improved survival in patients with pelvic fracture: Propensity score matching analyses. Eur J Trauma Emerg Surg 2021;47(6):1661–9.




6. Lee MA, Yu B, Lee J, Park JJ, Lee GJ, Choi KK, et al. Effects of the establishment of a trauma center and a new protocol on patients with hemodynamically unstable pelvic fractures at a single institution in Korea. Eur J Trauma Emerg Surg 2019;45(2):73–9.



7. Shim H, Jang JY, Kim JW, Ryu H, Jung PY, Kim S, et al. Effectiveness and postoperative wound infection of preperitoneal pelvic packing in patients with hemodynamic instability caused by pelvic fracture. PLO One 2018;13(11):e0206991.



8. Jang JY, Shim H, Kwon HY, Chung H, Jung PY, Kim S, et al. Improvement of outcomes in patients with pelvic fractures and hemodynamic instability after the establishment of a Korean regional trauma center. Eur J Trauma Emerg Surg 2019;45(1):107–13.



9. Bugaev N, Rattan R, Goodman M, Mukherjee K, Robinson BRH, McDonald AA, et al. Preperitoneal packing for pelvic fracture-associated hemorrhage: A systematic review, meta-analysis, and practice management guideline from the Eastern Association for the Surgery of Trauma. Am J Surg 2020;220(4):873–88.


10. Li Q, Dong J, Yang Y, Wang G, Wang Y, Liu P, et al. Retroperitoneal packing or angioembolization for haemorrhage control of pelvic fractures--Quasi-randomized clinical trial of 56 haemodynamically unstable patients with Injury Severity Score ≥33. Injury 2016;47(2):395–401.


11. Burlew CC, Moore EE, Stahel PF, Geddes AE, Wagenaar AE, Pieracci FM, et al. Preperitoneal pelvic packing reduces mortality in patients with life-threatening hemorrhage due to unstable pelvic fractures. J Trauma Acute Care Surg 2017;82(2):233–42.



12. Moskowitz EE, Burlew CC, Moore EE, Pieracci FM, Fox CJ, Campion EM, et al. Preperitoneal pelvic packing is effective for hemorrhage control in open pelvic fractures. Am J Surg 2018;215(4):675–7.


13. Petrone P, Rodríguez-Perdomo M, Pérez-Jiménez A, Ali F, Brathwaite CEM, Joseph DK. Pre-peritoneal pelvic packing for the management of life-threatening pelvic fractures. Eur J Trauma Emerg Surg 2019;45(3):417–21.



14. Salcedo ES, Brown IE, Corwin MT, Galante JM. Pelvic angioembolization in trauma - Indications and outcomes. Int J Surg 2016;33(Pt B):231–6.


15. Hundersmarck D, Hietbrink F, Leenen LPH, Heng M. Pelvic packing and angio-embolization after blunt pelvic trauma: A retrospective 18-year analysis. Injury 2021;52(4):946–55.


16. Morrison JJ, Galgon RE, Jansen JO, Cannon JW, Rasmussen TE, Eliason JL. A systematic review of the use of resuscitative endovascular balloon occlusion of the aorta in the management of hemorrhagic shock. J Trauma Acute Care Surg 2016;80(2):324–34.


17. Harfouche M, Inaba K, Cannon J, Seamon M, Moore E, Scalea T, et al. Patterns and outcomes of zone 3 REBOA use in the management of severe pelvic fractures: Results from the AAST Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery database. J Trauma Acute Care Surg 2021;90(4):659–65.


18. Lendrum R, Perkins Z, Chana M, Marsden M, Davenport R, Grier G, et al. Prehospital resuscitative endovascular balloon occlusion of the aorta (REBOA) for exsanguinating pelvic haemorrhage. Resuscitation 2019;135:6–13.


19. Pieper A, Thony F, Brun J, Rodière M, Boussat B, Arvieux C, et al. Resuscitative endovascular balloon occlusion of the aorta for pelvic blunt trauma and life-threatening hemorrhage: A 20-year experience in a Level I Trauma Center. J Trauma Acute Care Surg 2018;84(3):449–53.


20. Chang SW, Chun S, Lee G, Seo PW. Resuscitative endovascular balloon occlusion of the aorta for an iliac artery aneurysm: Case report. J Chest Surg 2021;54(5):429–32.



21. Cho S, Ryu JW, Chang SW. Resuscitative endovascular balloon occlusion of the aorta for retroperitoneal hemorrhage and shock after ipsilateral antegrade angioplasty with vascular closure device. Ann Transl Med 2020;8(6):404.



-
METRICS

-
- 1 Crossref
- 1,715 View
- 33 Download
-
Related articles in
J Acute Care Surg