Characteristics and Clinical Outcomes of Elderly Patients with Trauma Treated in a Local Trauma Center
Article information
Abstract
Purpose
This study aimed to investigate the characteristics of elderly patients who visited a non-regional trauma center to examine the effects of old age on the clinical outcomes of patients.
Methods
The medical charts of 159 patients with trauma who visited the National Health Insurance Service Ilsan Hospital between March 2020 and February 2022 were retrospectively analyzed.
Results
Of the 159 patients, 41 were assigned to the elderly patient group (EPG) and 118 were assigned to the non-elderly patient group (NEPG). The average age of patients in each group was 75.5 and 38.2 years in the EPG and the NEPG, respectively. Comparing the injury mechanism between the two groups, pedestrian traffic accidents (TA) were the most common (24.4%), followed by slipping (19.5%), motorcycle TA, and bicycle TA (14.6%) in EPG. In the NEPG, motorcycle TA (28.0%) was the most common, followed by car TA (27.1%), and fall injury (16.9%), with a significant difference between the two groups (p < 0.001). The significant differences between the two groups were the injury severity score (ISS; p = 0.004), severe trauma (p = 0.045), intensive care unit admission (p = 0.028), emergency operation (p = 0.034), and mortality (p = 0.013). The statistically significant risk factors for mortality were old age (p = 0.024) and chest injury (p = 0.013).
Conclusion
Patients in the EPG compared with the NEPG group showed different injury mechanisms. The EPG has a higher severity and mortality rate than the NEPG.
Introduction
The regional trauma center project was initiated by the Korean government in 2012, and the clinical outcomes of patients with trauma continues to improve, and the preventable trauma death rate (PTDR) has decreased to 21.4% in 2019 from 35.2% in 2010 [1]. Currently, there are 15 regional trauma centers operating, and regional trauma systems are being organized around them [2].
In 2020, Korea entered an aged society, with 15.7% of the population aged 65 years and older. The elderly population is more vulnerable to trauma than the younger population, and has a higher mortality rate for both major and minor trauma [3,4]. Although several studies on elderly patients with trauma have been reported in Korea, after the start of the regional trauma center project, studies on patients in hospitals other than regional trauma centers are limited [5,6].
The PTDR is higher in hospitals that are not regional trauma centers [1]. As the elderly population increases, we suspect the number of elderly trauma patients will increase. All patients cannot be treated by regional trauma centers and treatment data is very limited in non-regional trauma centers. Therefore, this study aimed to investigate the characteristics of elderly patients who visited non-regional trauma centers to examine the effects of old age on their clinical outcomes.
Materials and Methods
1. Study design and patient population
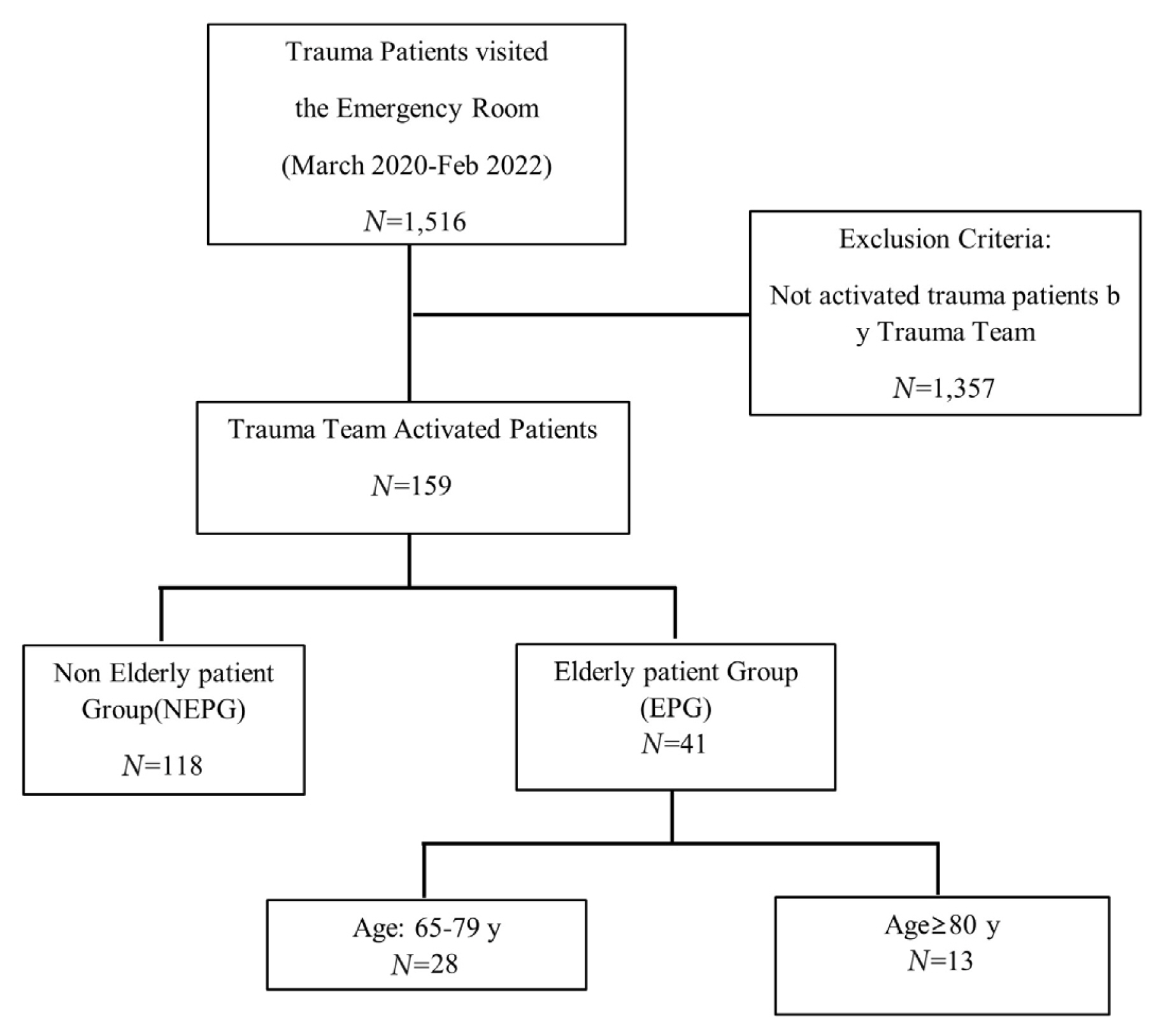
There were 1,516 trauma patients who visited the Emergency Room of a non-regional trauma center (National Health Insurance Service Ilsan Hospital) from March 2020 to February 2022. Out of these patients, only trauma team activated patients (n = 159) were included in the study. The medical charts of the 159 patients who were activated by trauma team were retrospectively analyzed. Patients were assigned to one of two groups according to age (65 years and older and under 65 years), the clinical characteristics between the two groups were compared, and the factors related to the patient’s death were identified as previously described [6,7]. In addition, a sub-analysis of the elderly group (65 years and older) was performed whereby the group was further divided into two groups: 65 to 79, and 80 years and older as previously described (Figure 1) [7]. An injury severity score of higher than 15 was defined as severe trauma in this study.
2. Outcome measurement
The primary objective of this study was to evaluate the effects of old age on the clinical outcomes of patients with trauma treated in a non-regional trauma center i.e., a local trauma center. The secondary outcome of this study was the assessment of the clinical characteristics of elderly patients with trauma. The data included age, sex, systolic blood pressure (SBP), Glasgow coma scale (GCS) score, injury mechanism, transfer to another hospital, abbreviated injury score (AIS), injury severity score (ISS), intensive care unit (ICU) admission, hospital stay, emergency operation, and in-hospital mortality.
3. The criteria for trauma team activation in the National Health Insurance Service Ilsan Hospital
The criteria for trauma team activation were divided into three categories: primary survey, secondary survey, and mechanism of the accident. During the primary survey if the patient had airway obstruction, or was intubated, the respiratory rate was lower than 10 or higher than 29, mental state was altered (GCS < 13), or the patient was transferred whilst receiving a blood transfusion, the trauma team was activated.
During the secondary survey, if there was penetrating trauma, flail chest, an open skull fracture, cord injury, pelvic fracture, two or more proximal long bone fractures or amputated limbs the trauma team was activated.
The mechanism of accident such as falling from a height of at least 6 meters, a crushed car of depth of more than 30 cm, if the patient was displaced from vehicle, death of a co-passenger, motorcycle or bicycle accident at a speed of more than 30 km/h, or a patient presenting with seat-belt injury after a vehicle accident would activate the trauma team.
4. Trauma system in the National Health Insurance Medical Center
The trauma team was composed of specialists in trauma surgery, emergency medicine, orthopedic surgery, neurosurgery, cardiothoracic surgery, and interventional radiology. When a patient arrives in the emergency room, is triaged, and meets the criteria to activate the trauma team, a text message is sent to the members of the trauma team. Emergency medicine physicians perform initial management such as initial resuscitation and focused assessment with sonography for trauma, and the trauma surgeon starts treating the patient within 30 minutes and decides the disposition.
In the event of trauma team activation, the computed tomography room and surgery-related department are collectively contacted to establish a pathway for emergency imaging, surgery, and radiological intervention as quickly as possible. Patients with multiple trauma are mainly admitted to the Department of Trauma Surgery, and acute treatment is performed in the emergency ICU. To meet the standards of the Level 3 trauma center of the American Association of Surgery of Trauma (AAST), an in-hospital trauma system was established, such as a trauma conference, panel discussion for trauma-related preventable death rate, and quality improvement activities [3].
5. Statistical analysis
Categorical variables were compared using the chi-square and Fisher’s exact tests. Continuous variables were compared using the student t test and Mann-Whitney U test. Logistic regression analysis was used to evaluate the risk factors associated with mortality, and the results were expressed as odds ratios (OR) with a 95% confidence interval (CI). Statistical significance was set at p < 0.05. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) Version 23 (IBM, Armonk, NY, USA).
Results
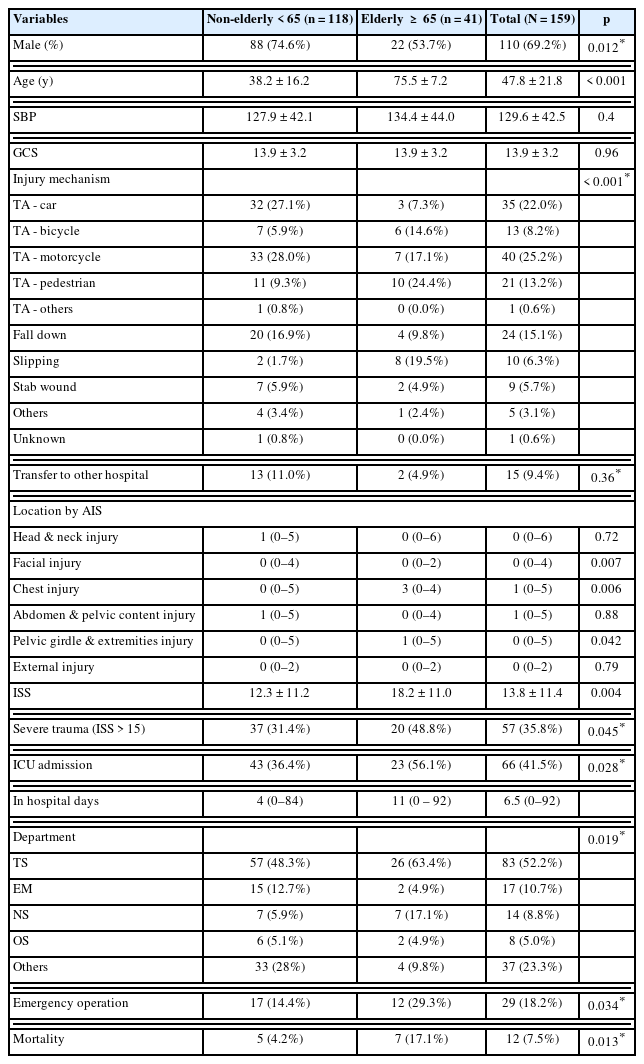
The mean age was 47.8 years, and 69.2% were men. Patients were assigned to one of two groups either the elderly patient group (EPG, 65 years and older) or the non-elderly patient group (NEPG), with 41, and 118 patients in each group, respectively. The average age of the EPG was 75.5 years, and 38.2 years in the NEPG (p < 0.001). In the EPG, the proportion of males was 53.7%, and in the NEPG it was 74.6% (p = 0.012). There was no significant difference in the initial SBP (p = 0.401) or GCS score (p = 0.959). Comparing the injury mechanism between the two groups, in the EPG pedestrian traffic accidents (TA) were the most common (24.4%), followed by slipping (19.5%), and motorcycle TA (17.1%). In the NEPG, motorcycle TA (28.0%) was the most common, followed by car TA (27.1%) and fall injury (16.9%). There was a significant difference between the injury mechanism between the two groups (p < 0.001). There was no significant difference in patient transfer (p = 0.357). The EPG scored significantly higher on the ISS (18.2 ± 11.0) than the NEPG (12.3 ± 11.2; p = 0.004). The EPG had a significantly higher proportion of patients with severe trauma (48.8 %) than the NEPG (35.8 %; p = 0.045). The EPG had a higher proportion of ICU admissions (56.1%) than the NEPG (36.4%; p = 0.028). In EPG, trauma surgery (TS) was the most common admission (63.4%), followed by neurosurgery (NS; 17.1%), and others (discharged or transferred, 9.8%). In the NEPG, TS (48.3%) was the largest, others were second with 28%, and third was emergency medicine (12.7%). The EPG had a significantly higher proportion of emergency operations (29.3%) than the NEPG (14.4%; p = 0.034). The EPG had more severe injury to the chest than NEPG [3, (0–4) vs 0, (0–5); p = 0.006]. Mortality was significantly higher in the EPG (17.1%) than in the NEPG (4.2%; p = 0.013; Table 1).
The characteristics of the survivors and non-survivors were analyzed to determine the risk factors for mortality in trauma patients. The non-survivor group had a higher proportion of the EPG (58.3% vs. 23.1%), lower SBP (76.3 ± 79.0 vs. 133.9 ± 35.2), and lower GCS (7.4 ± 5.6 vs. 14.5 ± 2.2). The severity of trauma for non-survivors had a higher ISS (33.5 ± 7.2 vs. 12.2 ± 10.1), and the proportion of severe trauma was significantly higher (100% vs. 30.6%). The severity of injury to location using the AIS, showed a higher median value for chest injury in the non-survivor group than in the survivor group [3, (0–4) vs 0, (0–5); p < 0.001]. However, there was no statistically significant difference in the proportion of patients admitted to the ICU or those who underwent an emergency operation (Table 2).
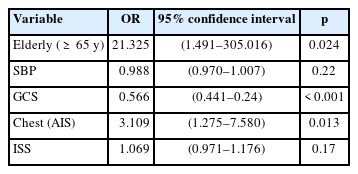
The risk factors associated with mortality were measured using logistic regression with variables that were statistically significant in the univariate analysis. The independent risk factors were old age (OR 21.315, 95% CI 1.491–305.016), and chest injury (AIS 3; OR 3.109, 95% CI 1.275–7.580). The patients had a higher probability of survival when they had a high GCS initially (OR 0.566, 95% CI 0.441–0.24; Table 3).
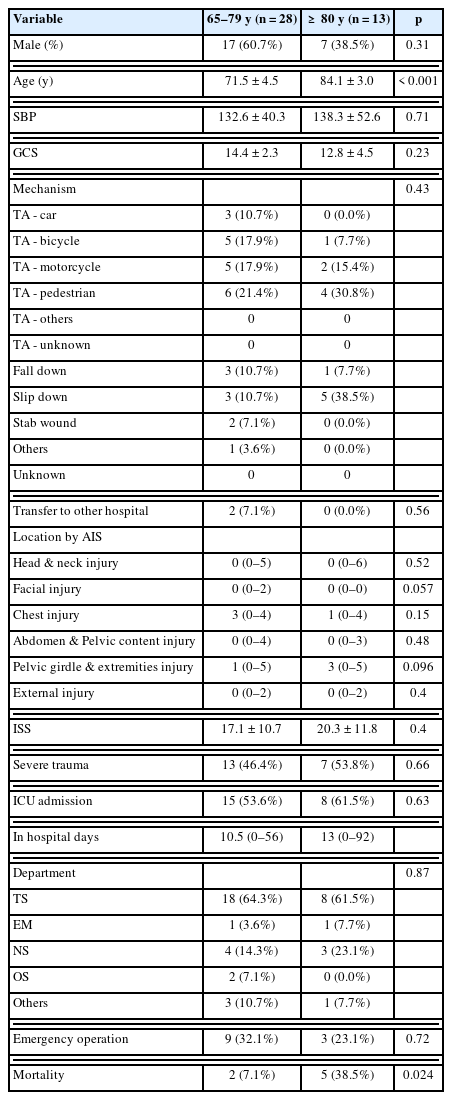
A subgroup analysis of the EPG (65–79 years and 80 years or older) was performed to determine whether there were different characteristics. The two groups were similar in most characteristics, except mortality where the 65–79 group had 7.1% mortality, and the 80 years and older group was 38.5% (p = 0.024; Table 4).
Discussion
In this retrospective study the ratios of injury mechanisms were high for pedestrian TA and slipping in the EPG, whereas in-car TA, motorcycle TA, and fall from height were relatively low. This result is similar to a study In the United States, where ground-level falls accounted for the most common mechanism of injury (2.1 million) presenting in the emergency department in 2008, and similarly this was 10 times more common than the second leading cause of trauma in the elderly which was motor vehicle crashes (8). Another study reported that 6% of elderly patients with ground-level falls experienced a fracture, 10–30% had multiple traumas, and the mortality rate was 7% (9)]. In addition, in this current study, the EPG had a higher ISS than that of the NEPG, were more commonly admitted to the ICU, and underwent emergency surgery more frequently. This is probably because elderly patients have a low physiological reserve and may have complicated underlying disease, and therefore, more damage occurs even with a small external force [10–13]. In addition, it was determined that old age (65 years and older) itself is a factor that increases the risk of death by approximately 21 times compared with patients aged less than 65 years (Table 3). In a sub-analysis of patients aged 80 years and older and 65–79 years, the mortality rate was significantly higher in patients aged 80 years and older, despite similar clinical characteristics (38.5% vs. 7.1%, p = 0.024). These results indirectly show that a patient’s tolerance to trauma continues to decrease with increasing age, even amongst elderly patients 65 years and above. Previous studies have identified these changes, and determined that changes in the cardiovascular and pulmonary systems have the greatest impact on patient’s prognosis [14,15]. In this current study the GCS and chest injury were independent risk factors of mortality which is similar to previous studies [9,16].
In Korea, the PTDR has continued to decrease, falling from 35.2% in 2012 to 30.5% in 2015, and the PTDR in 2017 dropped significantly to 19.9% [1,17]. In addition, national-scale data have shown that the actual mortality rate of patients with trauma has been decreasing since the start of the regional trauma center project, but the transfer rate increases each year [17]. This shows that injured patients fill the trauma centers, and regional trauma centers play a role as the ultimate treatment centers for patients with trauma [17]. A recent trauma mortality review in Gyeonggi-do showed similar results to this current study with an overall PTDR of 17.0%, but the stage where the most problems affecting preventable trauma death occurred was the hospital stage (86.7%), and most PTDR occurred in hospitals other than regional trauma centers. This suggests that improving the treatment process in non-regional trauma centers will improve the overall clinical outcomes of patients with trauma in Korea [2]. Local trauma centers could reduce the PTDR by investing systematically and clinically. If a trauma surgeon is hired, they will interact with other departments and can change the view of managing trauma patients by applying transfusion protocols, preventable death panel reviews, and trauma conferences. Clinically, prompt hemostasis of bleeding and transfusion will reduce the PTDR because delayed bleeding control is the most common error in PTDR. This can also lead to a reduction of the PTDR of inter-hospital transfer to regional trauma centers [2,18–20].
Since 2020, the National Health Insurance Service Ilsan Hospital became a Level 3 trauma center (using AAST criteria) with an in-hospital trauma system providing the resources necessary to give optimal care as set out by the AAST [21]. In particular, patients with trauma who were unable to be transported to the regional trauma center within 45 minutes of their injury or patients who required prompt initial management, such as airway management, resuscitation, and transfusion, were transported to the National Health Insurance Medical Center because of their serious condition.
When visiting all suspected severe trauma patients, the trauma team is activated, and the trauma surgeon becomes the team leader and makes decisions regarding the patient’s definitive care and disposition. A panel discussion enables assessment for the use of the PTDR as a quality improvement activity for the treatment of patients with severe trauma in the hospital. Several studies have reported that regional trauma centers have improved the clinical outcomes of severe trauma patients over approximately 10 years since the start of the regional trauma center project, but prehospital errors still persist, and there are many problems in the treatment of trauma patients in nonregional trauma centers [1,2,17,18,22,23]. This suggests that a more sophisticated trauma care system is needed through the configuration of a Korean Level 2 center (Level 3 by the AAST criteria) suitable for the characteristics of each region, in addition to the operation of regional trauma centers.
This study had several limitations. Firstly, as a single-center study, a relatively small number of patients were included in this review, in particular, the number of the EPG was very small. Secondly, selection bias was inevitable because this was a retrospective study. Nevertheless, it is a rare domestic study that shows the clinical characteristics of elderly patients and the initial experiences of staff at a local trauma hospital equipped with trauma systems.
Conclusion
In conclusion, patients in the EPG compared with the NEPG group showed different injury mechanisms. The EPG has a higher severity and mortality rate than the NEPG. Therefore, caution is needed in the treatment of elderly patients with trauma. In the future, a multicenter prospective study is required.
Notes
Author Contributions
Conceptualization: JYJ. Methodology: JYJ and KP. Formal investigation: KP, SL and KYL. Data analysis: KP, GC, SL and KYL. Writing original draft: KP and GC. Writing - review and editing: KP and JYJ.
Conflicts of Interest
Ji Young Jang has been the associate editor of Journal of Acute Care Surgery since March 2017, but had no role in the decision to publish this original article. There were no other potential conflicts of interest relevant to this article.
Ethical Statement
This research did not involve any human or animal experiments.
Data Availability
All relevant data are included in this manuscript.
Funding
This work was supported by National Health Insurance Service Ilsan Hospital grant NHIMC-2022-CR-035.