Case Report of an Appendiceal Mucinous Neoplasm: A Rare Etiology for Appendicitis
Article information
Abstract
An appendiceal mucinous neoplasm is a rare condition with a clinical picture that can resemble appendicitis. Published reports have documented an incidence of 0.07–0.3% of all appendicectomies. The ubiquitous use of computerized tomography scans has helped plan surgical strategies as these patients may often require a right hemicolectomy in order to ascertain oncological clearance. This helps the clinician to avoid the complication of pseudomyxoma peritonei with its attendant increased mortality. In this case report the presence of a normal appendix base allowed for a laparoscopic intervention without having to resect the right hemi-colon. All published case reports to date have documented the involvement of the entire appendix. This case report is unique in the sparing of the proximal appendix.
Introduction
An appendiceal mucocele, first described in 1842 by Rokitansky [1] is an outdated nomenclature. Current classification refers to appendiceal mucinous neoplasms. They can be benign or malignant. The epidemiology skews in favor of females in the 5th and 6th decades of life. Computerized tomography remains the gold standard for diagnosis of an appendiceal mucinous neoplasm and an appendix width of greater than 15 mm has an 83% sensitivity and 92% specificity for diagnosis [1]. This case report is unique as the pathology presents in a male patient in his 6th decade of life.
Case Report
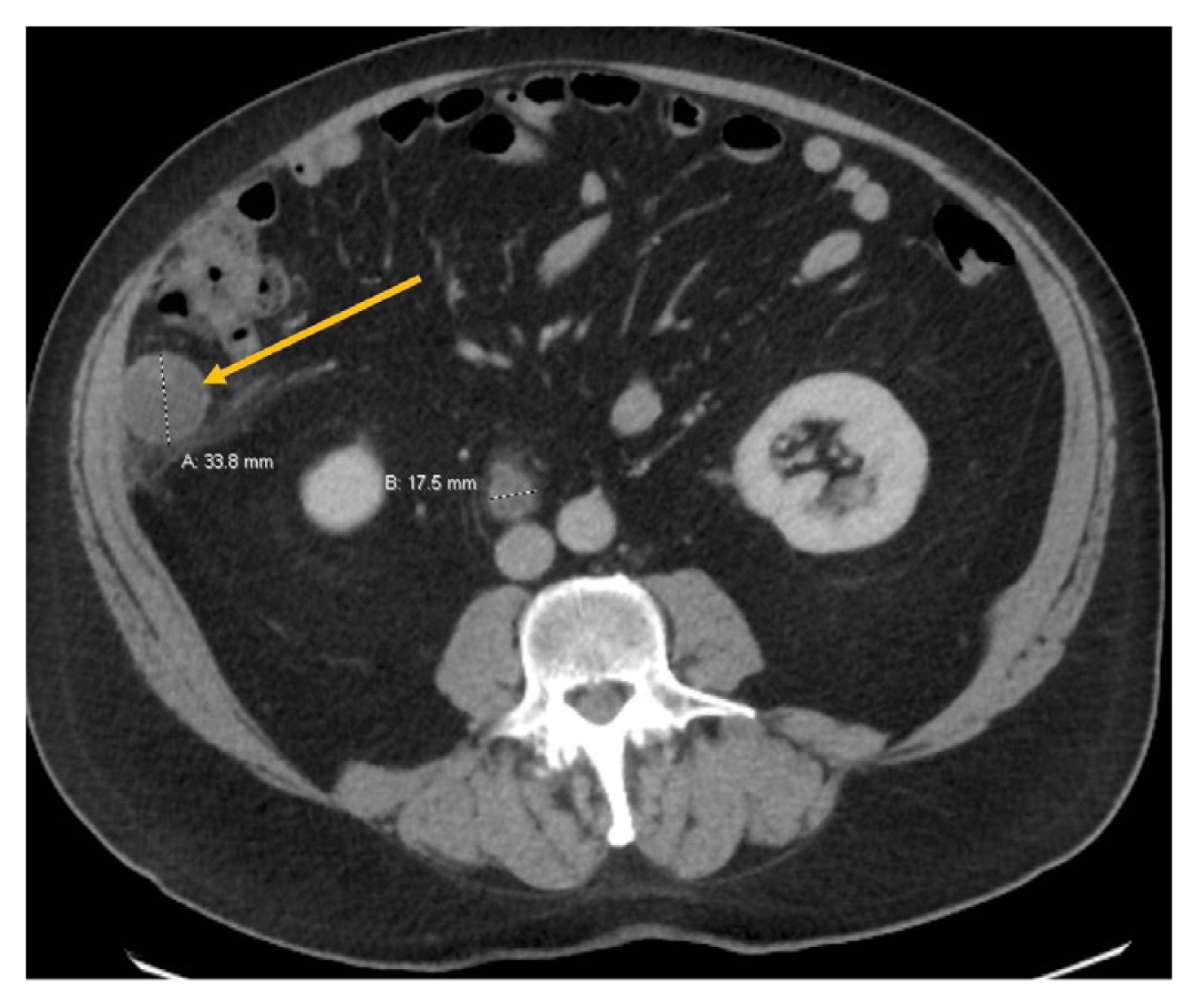
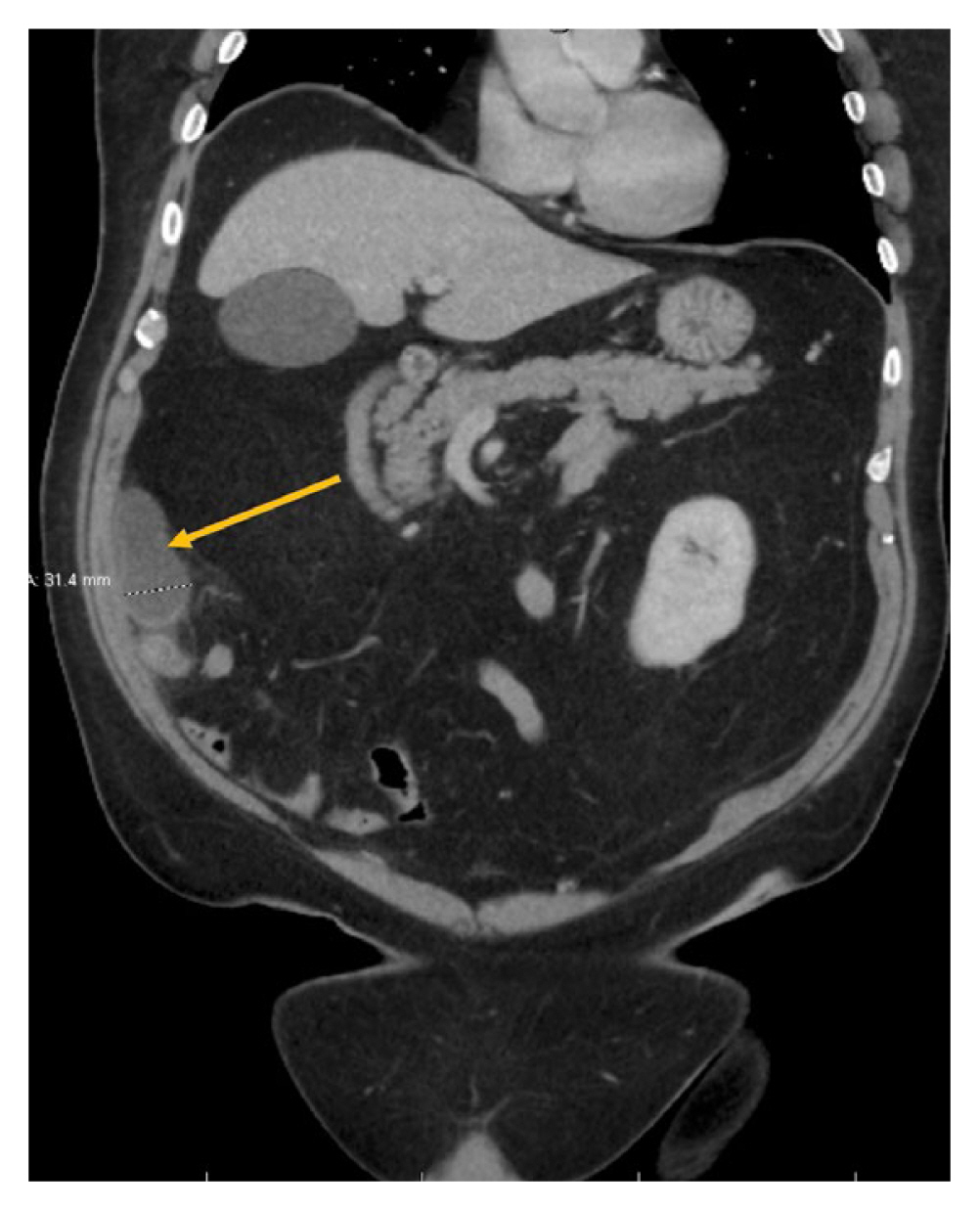
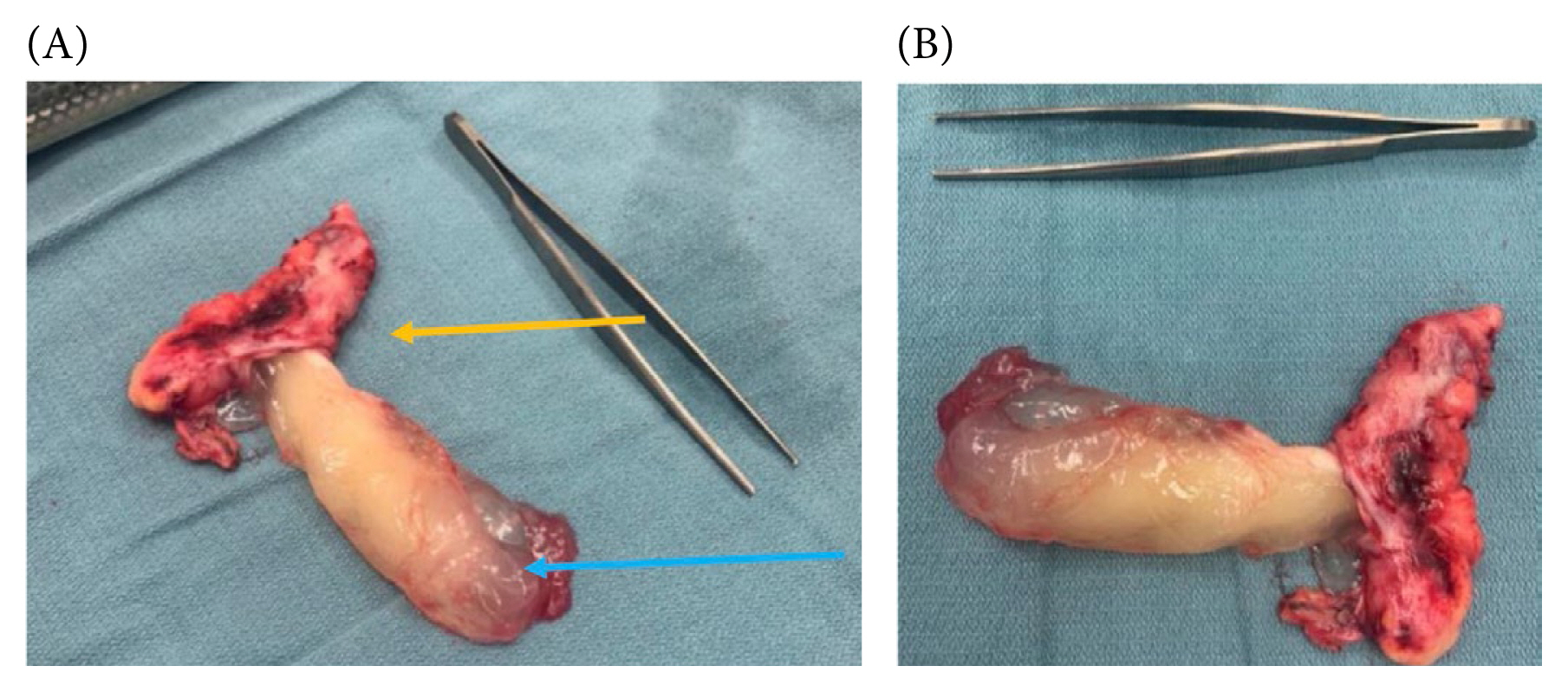
A 67-year-old male patient was referred to the Department of Acute Care Surgery for a possible acute appendicitis. He had a 2-day history of right lower quadrant pain in his abdomen. This was his first episode of right lower quadrant pain. There was no nausea, vomiting, fever or chills. Clinically, tenderness was elicited at the McBurney’s point but no signs of rebound tenderness or voluntary guarding were observed. He remained hemodynamically stable throughout following admission. Laboratory investigations showed a white cell count of 10,000 cells/μL and a C-reactive protein of 11 mg/L. Serum electrolytes were within normal parameters and urine chemistry was normal. Computerized tomography scan of the abdomen showed acute appendicitis with a 3.1 cm thick distal appendix (Figure 1). The appendix base was normal but contained a fecalith (Figures 2 and 3). After informed signed consent was given, he was taken to surgery and had a laparoscopic appendicectomy. We also discussed the possibility of further surgical intervention such as a right hemicolectomy due to the possibility of appendix malignancy. Intra-operatively the appendix was quite distended and difficult to grasp (Figure 4). The proximal 2 cm of the appendix was normal (Figure 5A) and we were able to grasp it and apply 2 ENDOLOOP’s to the appendix base (Figure 5B). There was iatrogenic bleeding from the appendicular artery stump, and this was secured with metallic gallbladder clips and an ENDOLOOP for adequate hemostasis. The patient made a routine recovery and was discharged home after 48 hours. Pathology confirmed a benign mucinous appendix neoplasm with no obvious meso-appendicular lymphadenopathy (Figures 6A and 6B). The appendix base was not involved in the mucinous neoplasm. At his 2 weeks follow up the diagnosis was discussed with the patient, and given his age as well as the diagnosis he consented to a colonoscopy. His colonoscopy 6 weeks later was normal.

Computerized tomography scan sagittal view showing the distended distal appendix (orange arrow) and with a normal base (green arrow), and appendicolith within.

(A) Normal appendix base (blue arrow) with distended distal appendix (green arrow); (B) Application of ENDOLOOP around the appendix base (blue arrow) with distended distal appendix (green arrow).
Discussion
An appendiceal mucinous neoplasm is defined as the abnormal accumulation of mucous within the appendiceal lumen [2,3]. This accumulation may involve an obstruction or a mucous secreting neoplasm. The etiological spectrum of an appendiceal mucinous neoplasm includes mucosal hyperplasia, retention cysts, mucinous cystadenomas, and mucinous cystadenocarcinomas [4,5] and it has an incidence of 0.07–0.3% of appendectomies [4,6]. Presentation is varied and 50% of patients are often asymptomatic [7]. Symptomatic patients can present with acute or chronic right lower quadrant pain, a palpable mass, mechanical obstruction, genitourinary symptoms, an acute abdomen, or sepsis [8].
The surgical management depends on the extent of the lesion. In the case of benign lesions such as cystadenomas and hyperplastic lesions, an appendectomy can be curative [1,9]. Complex or malignant neoplasms, such as a mucinous cystadenocarcinoma, require a right hemicolectomy [9] to achieve an oncological resection. If the base of the appendix is involved in the malignancy process which inhibits a surgeon’s ability to obtain a clear oncological margin, a more extensive resection such as an ileocecectomy or a right hemicolectomy can be performed.
Controversy has arisen over the decades in open versus laparoscopic appendicectomy in cases of localized mucinous neoplasms of the appendix. Moreno et al [4] recommended that mucinous lesions of the appendix should be removed via an open appendicectomy due to concerns of peritoneal seeding. This could lead to pseudomyxoma peritonei, which can be fatal [3,5]. A multicenter retrospective study reported that there was no statistically significant difference between open and laparoscopic techniques when comparing intraoperative rupture of the mucinous neoplasm [7]. Laparoscopic excision did not increase recurrence rates [1]. Laparoscopic appendicectomy appears to be a reasonable approach for removal of localized mucinous neoplasms. The presence of a normal appendix base of 2 cm contributed to our decision-making process in performing a laparoscopic appendiceal excision. Due to the strong relationship between colorectal malignancies and mucinous neoplasms the patient also had a colonoscopy 6 weeks later [10]. There is a reported incidence of a 20% risk of colorectal malignancies in patients with appendiceal mucinous neoplasms [10]. We believe this is the first case report with a normal appendix base and a distal mucinous neoplasm. All reported cases to date have involved the entire appendix including the base of the appendix.
Notes
Author Contributions
Conceptualization, primary surgeon, introduction, abstract and figures: YP. Discussion, referencing and editing: OB.
Conflicts of Interest
The authors declare that they have no competing interests.
Funding
None.
Ethical Statement
We acknowledge the permission of the patient who gave written consent for publication of his operative images.
Data Availability
All relevant data are included in this manuscript.