Introduction
Urinary bladder injuries represent 1.6% of blunt abdominal trauma cases [1]. The repair of traumatic intraperitoneal bladder rupture (TIBR) can be safely performed using laparoscopy in patients who are hemodynamically stable, and deliver favorable outcomes even in those with multiple extra-abdominal injuries [2]. We report 3 cases of TIBR at the bladder dome which were successfully repaired by a single surgeon, using laparoscopy. Moreover, several laparoscopic techniques were introduced, such as effective methods for bladder traction which facilitated a successful laparoscopic repair of TIBR.
Case Report
1. Cases
1.1. Case 1
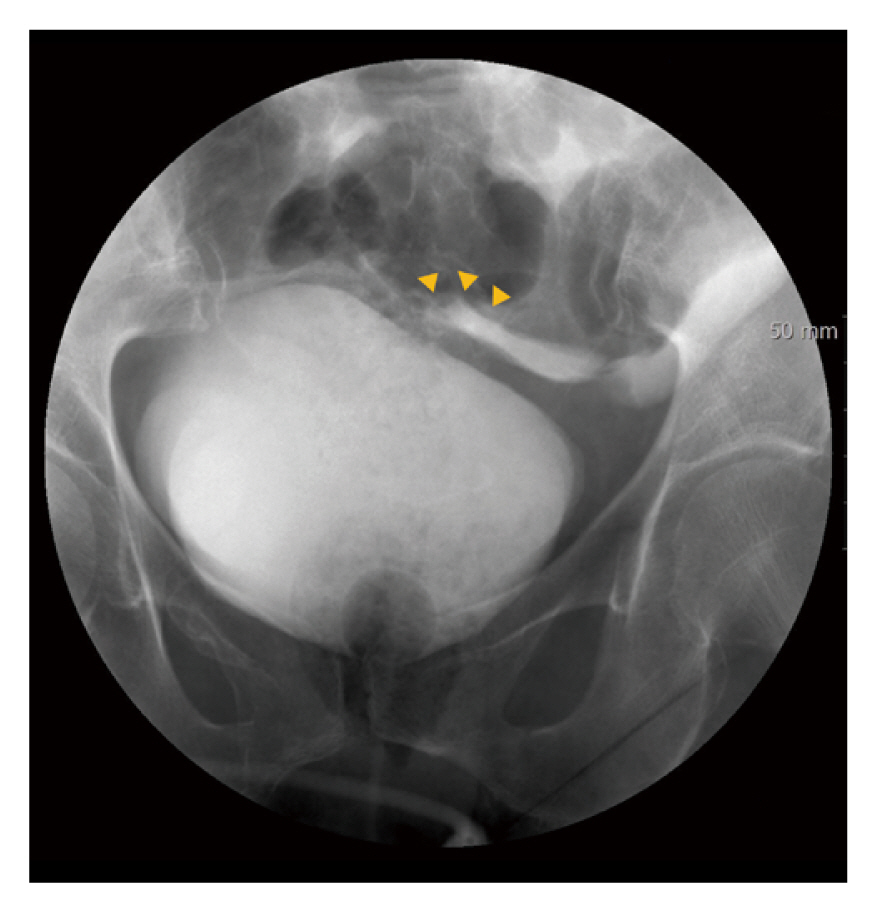
A 59-year-old female patient was admitted to the emergency room (ER) after being hit by an automobile. She was hemodynamically stable upon arrival. Physical examination revealed tenderness in the lower abdomen without peritoneal signs. The focused assessment with sonography for trauma examination was positive for fluid collection in the Morison’s pouch, splenorenal recess, and Douglas’ pouch. An abdominopelvic computed tomography (APCT) scan showed pubic rami fractures; however, the source of hemoperitoneum was undetermined. Mild hematuria was noted, and subsequently she was diagnosed with TIBR based on retrograde cystography (Figure 1). A linear tear measuring 5 cm at the dome of the bladder was repaired using laparoscopy without any complications.
1.2. Case 2
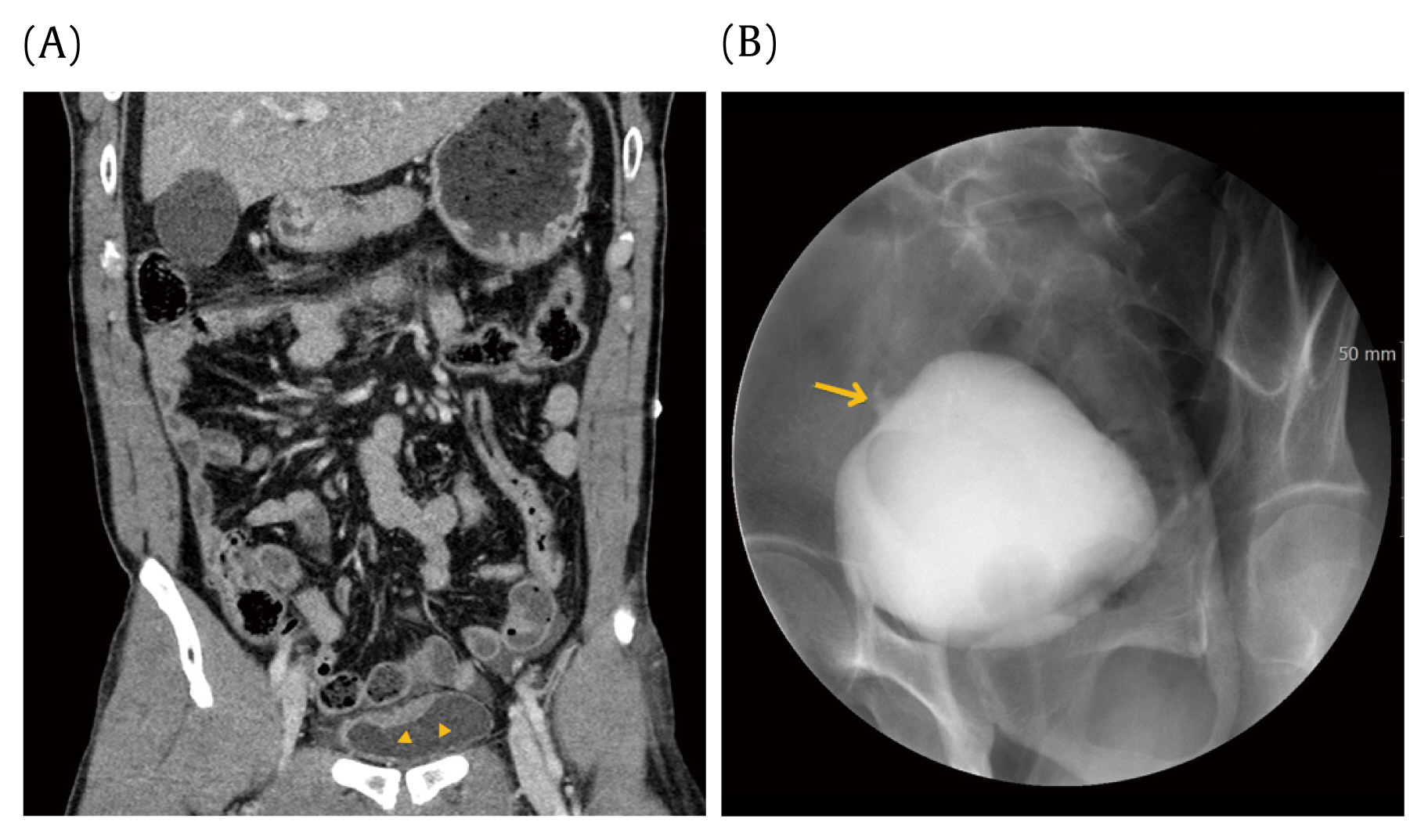
A 57-year-old male patient who was a driver involved in a high-velocity motor vehicle accident was admitted to the ER. He was hemodynamically stable and initially complained of lower abdominal pain. After a couple of hours, this pain was completely relieved. The abdominal examination showed no tenderness; however, the focused assessment with sonography for trauma scan was positive for fluid collection in the Morison’s pouch and rectovesical pouch. Foley’s catheter was inserted and revealed gross hematuria. The APCT scan showed a thick-walled bladder dome; however, retrograde cystography showed no contrast leakage (Figures 2A and B). As there was no tenderness in the abdomen and bowel sounds were normal, the Foley’s catheter was removed after 2 days. However, he developed urinary retention; thus, Foley’s catheter was reinserted, and signs of peritoneal irritation were observed immediately. The repeat APCT scan showed that the Foley’s catheter had penetrated the bladder wall (Figure 2C). An exploratory laparoscopy showed a vertical laceration of 6 cm at the dome of the bladder with the Foley’s catheter balloon floating freely in the peritoneal cavity. The laceration was completely closed with laparoscopic suturing.
1.3. Case 3
A 48-year-old male patient was admitted to the ER after being hit by a motor vehicle. His vital signs were stable and gross hematuria was observed. Similarly, his APCT scan revealed a thick-walled bladder dome, and based on the cystogram, he was diagnosed with isolated TIBR (Figures 3A and B). The 4 cm injury was repaired laparoscopically.
2. Surgical technique
Following peritoneal access using a 10 mm supraumbilical camera port, 2 working ports measuring 5 mm were placed in both iliac fossae. Then, a traction stitch was made at the cranial or caudal end of the bladder laceration for bladder fixation. The interior of the bladder was examined using a laparoscope to check if both ureteral orifices were intact. A double-layer closure was performed with intracorporeal suturing using 3-0 barbed sutures (V-Loc 90 absorbable device, Covidien, Minneapolis, MN, USA). Then, indigo carmine diluted with 300 mL saline was instilled into the bladder via a Foley’s catheter to check if there were any leakages. A Jackson-Pratt drain was placed in the retropubic space. The drain was removed on postoperative Day 3 if the content was serous and minimal. A 3-way indwelling Foley’s catheter with continuous normal saline irrigation was applied until blood clots were resolved. On postoperative Day 7, the Foley’s catheter was removed after a negative cystogram result.
Discussion
Bladder injuries are classified into 5 patterns: Type 1 - bladder contusion; Type 2 - intraperitoneal rupture; Type 3 - interstitial rupture; Type 4 - extraperitoneal rupture; and Type 5 - combined intra- and extraperitoneal rupture [3]. The 3 patients in this case series had injuries to the bladder dome which were Type 2. The bladder dome is most likely to tear as a result of high energy blunt trauma to the lower abdomen of a patient with a distended bladder because it is the weakest part of the bladder anatomically [4].
This case series presents the safety and potential superiority of laparoscopic repair of TIBR. A previous retrospective review reported the advantages of laparoscopic bladder repair compared with open repair [2], such as a shorter hospital stay and a lower risk of abdominal complications including adhesive bowel obstruction, and incisional hernia. In this current case series, the patients did not experience abdominal complications. The average length of hospital stay was 23 days, which was longer than that in previous reports, due to concomitant traumatic injuries in Cases 1 and 3.
In Case 2, the diagnosis of TIBR was delayed. Bladder injuries can be missed in patients with multitrauma because the symptoms can be nonspecific and vague in the early stages and often attention is directed to other life-threatening injuries. Delayed diagnosis of bladder rupture is associated with significant morbidity and mortality rates [3]. Unfortunately, in this patient, there was no constant abdominal pain or decrease in urinary volume, and retrograde cystography failed to detect leakage of dye. However, in a retrospective review, findings from the APCT scan suggested TIBR (Figures 2A and B). Although rare, clinicians should have a high index of suspicion of TIBR in trauma patients with unexplained abdominal findings despite negative cystography results.
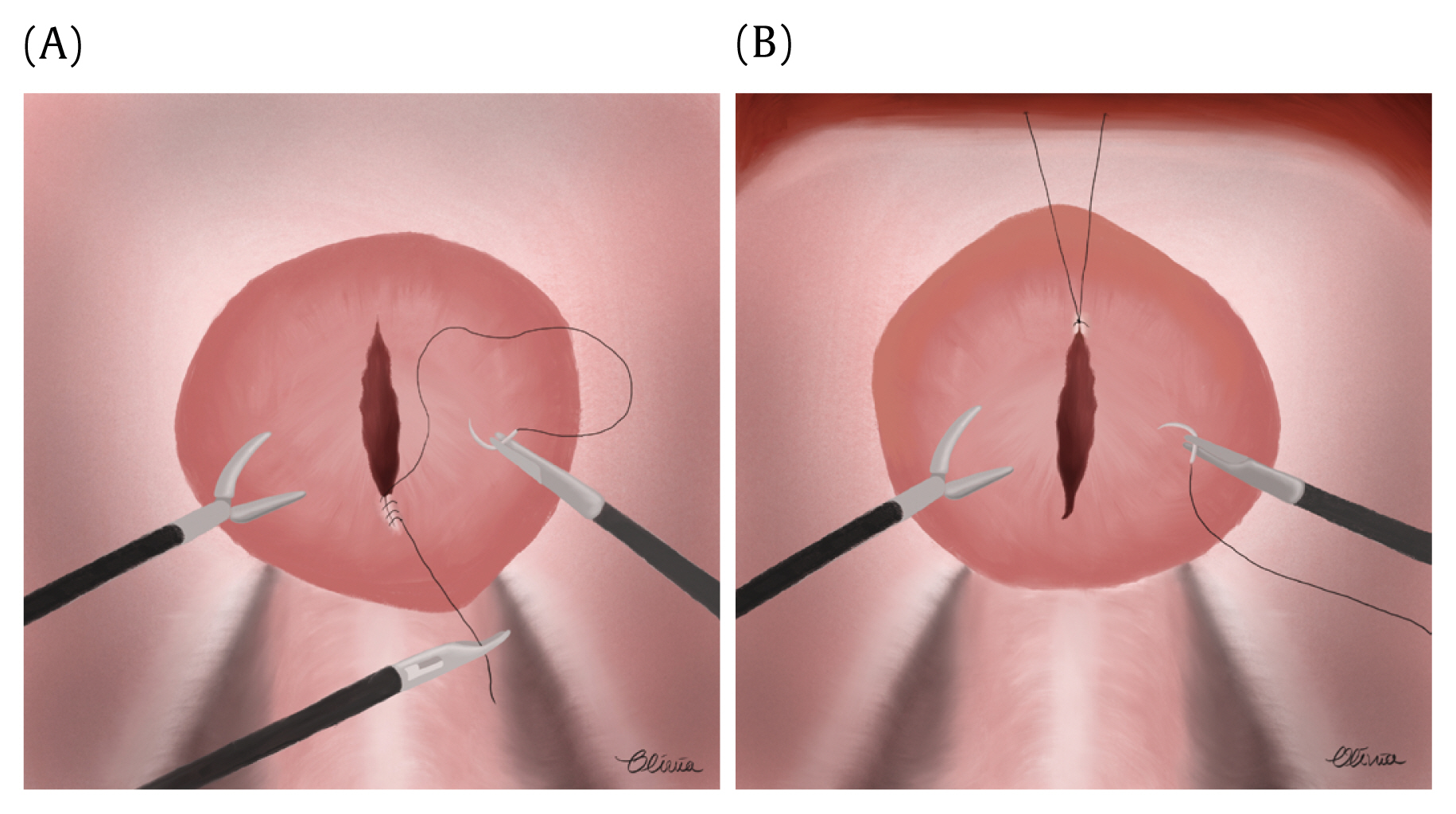
There were several points of surgical techniques that should be highlighted in the laparoscopic repair of TIBR. Before cystorrhaphy is performed, the trigone of the urinary bladder, including the integrity of ureteral orifices, should be inspected laparoscopically and repaired if injured. A single-layer or double-layer closure of TIBR should be performed with absorbable sutures, using either a continuous or interrupted technique [2,5,6]. Although the repair principles of the 3 cases were the same, techniques for traction of the bladder varied. In Cases 1 and 3, the dorsal end of the bladder laceration was pulled by 5 mm and 2 mm assistant graspers, respectively (Figure 4A). Then, freehand suturing was performed from the bottom upwards. In Case 2, a suspension suture at the ventral end of the laceration was made through the skin using a suture passer, and a downward intracorporeal suture was performed (Figure 4B). In our experience, surgical fluency of suturing depends on whether the surgeon chooses the correct direction of traction when working in difficult angles. In this regard, traction by an assistant grasper facilitates suturing compared with the immobile suspension suture to the abdominal wall. The watertight seal should be checked by instillation of normal saline, methylene blue, or indigo carmine into the bladder intraoperatively; and by conventional cystography 7–14 days postoperatively [2,5,6].
Intracorporeal suturing and exploratory laparoscopy to address other possible concomitant injuries are the minimal surgical techniques required to perform a successful laparoscopic repair of TIBR. However, prudent, and timely selection of candidates is important. We hope that this case report promotes the use of laparoscopic cystorrhaphy among trauma surgeons.