Introduction
Stab wounds to the neck are potentially lethal and often associated with vascular injury of the carotid artery and jugular vein. Simultaneous penetrating injuries to the carotid and vertebral arteries are uncommon, potentially causing severe bleeding and neurological deficits. We report a case of simultaneous carotid and vertebral artery transection managed by surgery and interventional angioembolization.
Case Report
A 30-year-old male with no history of illness presented to the Emergency Department after receiving a stab wound to the left neck area. Ambulance paramedics reported profuse bleeding from the neck when they arrived on the scene. The primary survey revealed a drunken, semi-comatose patient with normal sounds of breathing. Vital signs showed blood pressure which could not be measured, and tachycardia of 117 beats per minute on electrocardiogram monitoring. Initial volume resuscitation was started. A complete physical examination revealed an anteromedial stab wound to the left side of his neck with active bleeding. The internal, external, and common carotid arteries were completely transected, as was the internal jugular vein. The proximal and distal stumps of these vessels were clamped in the Emergency Room (Figure 1). Soon after, the systolic blood pressure was maintained above 90mmHg. The patient was taken to the Operating Room where, under the exploration of the left side of the neck, the carotid arteries were repaired by interposition saphenous vein grafting, and the internal jugular vein was ligated. It took about 3 hours from neck injury to revascularization of carotid artery. However, there was arterial bleeding from a deeper portion, and the source
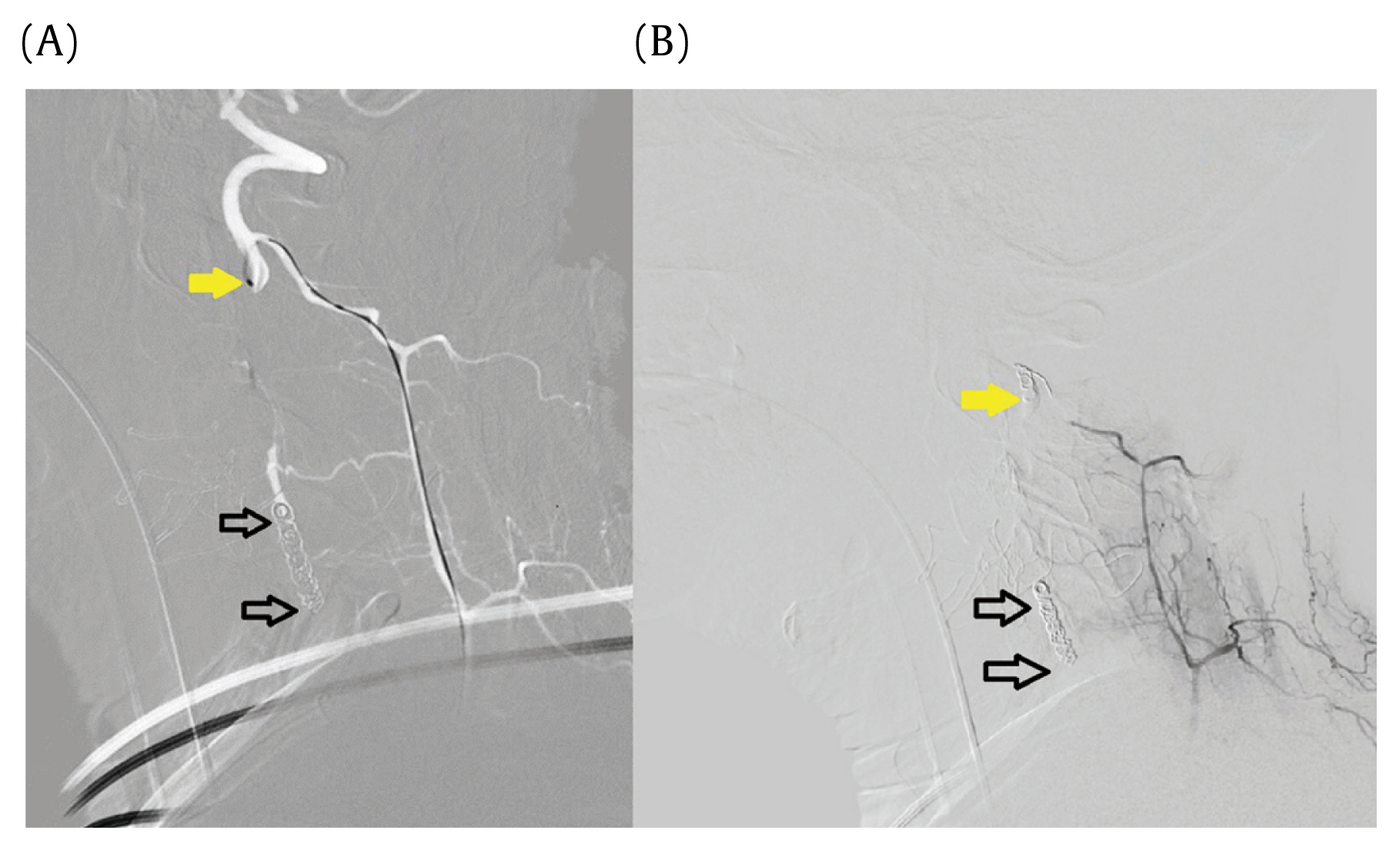
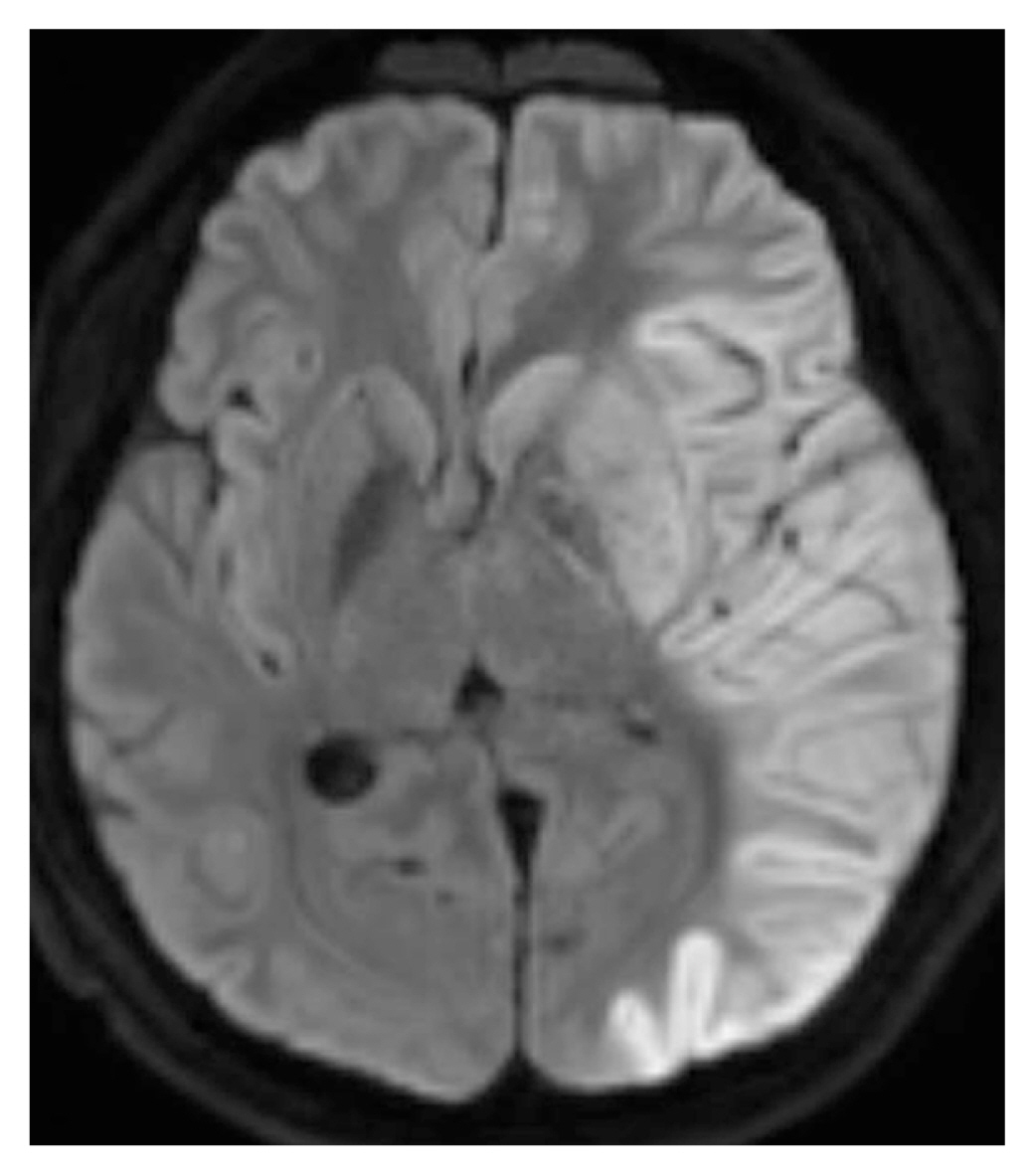
was the transverse foramen of the cervical spine. Thus, the patient was taken to the intervention room for an angiogram, which showed discontinuation of the left mid-cervical vertebral artery (Figures 2A and 2B). This area was the bleeding focus, and embolization was performed by an interventional radiologist (Figures 3A and 3B). After the vital signs stabilized, the neck muscles and wounds were repaired. On postoperative Day 2, the patient opened his eyes but could not make eye contact and did not obey instruction. On postoperative Day 3, a follow-up magnetic resonance imaging scan revealed extensive cortical acute infarct involving most of the anterior cerebral artery and middle cerebral artery territories with herniation but no hemorrhagic transformation (Figures 4 and 5). After performing the magnetic resonance imaging scan, tonic seizures occurred, and his eyeball deviated upward and to the left prompting a consultation with neurosurgery which resulted in the patient receiving coma therapy. On postoperative Day 10, the patient’s eyes opened in response to pain stimulus, and right-sided weaknesses were observed. The patient was extubated on the same day but presented with global aphagia. Motor examination revealed Grade 2/5 strength in his right arm and 1/5 in his right leg. Following rehabilitation, the patient was discharged on postoperative Day 52. When the patient visited the Outpatient Department on postoperative Day 59, global aphagia was still observed, but motor examination revealed Grade 3/5 strength in his right arm and 4/5 in his right leg.
Discussion
Carotid artery injuries are associated with high mortality (50%) and persistent neurological deficits (80%). Most patients with vascular neck injury died where the injury occurred or during transportation to the hospital. The usual pathology of neurological deficit following vascular neck injury is ischemic cerebral infarction caused by hypoperfusion or thromboembolism [1,2].
When examining a patient with injury to the vascular neck, it is important to check for “hard signs.” Hard signs are reliable indicators for carotid artery injury and include an expanding or pulsatile hematoma, the absence of a pulse, the presence of bruit, and active external bleeding. Hemodynamically stable patients can be clinically observed and evaluated using radiological investigations [3]. Computed tomography angiography is the initial and the most informative diagnostic tool for patients with penetrating neck injuries who do not present with hard signs [4]. Noninvasive imaging such as magnetic resonance (MR) with angiography is also useful in the initial diagnosis and follow-up [5]. When carotid artery injury is suspected, and diagnostic procedures are impossible, then exploratory surgery is justified [1]. In this Case Report, the exploratory surgery was performed immediately without an evaluation using imaging because the patient’s condition was unstable.
The mainstay of treatment should be early and aggressive resuscitation and revascularization. Patients undergoing revascularization generally benefit compared with patients who undergo ligation. The pathological basis is based on the principle of reperfusion of marginally perfused cerebral tissue. The recruitment of ischemic penumbra to normally functioning neurological tissue results in a better neurological outcome [2,6]. Thus, revascularization should be attempted whenever possible, regardless of the threat of hemorrhagic infarction, because hemorrhagic infarction rarely occurs and is unpredictable. Subsequent ischemic or hemorrhagic cerebral infarction are also unpredictable; the overall outcome of revascularizing the injured artery is superior to that achieved with ligation [1,2,7].
The literature indicates that revascularization should be attempted in all patients, even those in a coma [8–10]. Immediate revascularization of coma patients appears to offer the best chance of improvement. A depressed mental status may be caused by shock, hypoxia, sedation, paralysis for airway control, or a combination of these [1,7]. The patient who is comatose and in profound shock should be treated like their neurological function will return to normal if the bleeding is controlled, blood volume restored, and the carotid artery injury promptly repaired [11]. Likewise, our patient had some improvement in neurological function after the critical period.
There are surgical or endovascular revascularization methods which are possible for vascular neck injury. However, surgical revascularization remains the gold standard for managing carotid artery transections, which can be performed by end-to-end anastomosis, lateral sutures, and patch repair or bypass grafting (for larger injuries) [12,13]. Surgeons must consider during surgery that patients should be routinely draped for saphenous vein harvest. In patients with an incomplete circle of Willis, special attention should be paid to reduce ischemic infarction due to hypoperfusion during clamping and thromboembolism during surgical manipulation [2]. After achieving proximal and distal control, together with heparinization, visible thrombi should be carefully removed. Back-bleeding from the distal injured vessel indicates repair. Although shunting may decrease the ischemia duration, shunts may inherently increase thromboembolic events [2].
An extracranial internal carotid artery injury can be surgically challenging and occasionally requires ligation to prevent exsanguination. When ligation is performed, stroke and mortality rates are higher [1], likely related to the absence of collateral flow when the vessel is damaged or clamped, especially in patients with an incomplete circle of Willis and inaccessible bleeding in distal injuries. Variants in the circle of Willis anatomy are very common, with only 20% of patients (in anatomical studies) having a complete circle without any hypoplastic segments. In a trauma setting, having normal cerebral vascular anatomy is not enough to protect against a patient having a stroke [14]. Therefore, the indications for carotid artery ligation should be limited to the following circumstances: a very severe condition in the patient, a severe brain injury not associated with the carotid artery injury (e.g., a gunshot wound in the brain), a high Zone 3 internal carotid artery injury in the base of the skull when an anastomosis is not possible, and extensive distal-internal carotid artery thrombosis. In all other cases, the surgery should be restoration of carotid patency [1,7].
Endovascular therapy safely and effectively restores vascular luminal continuity or embolization if the surgical exposure is complicated [4,5]. The deep location of the vertebral artery within the neck makes injury relatively less common. However, this location also makes it difficult to detect and manage [15]. Additionally, a vertebral artery injury is surgically challenging because it is difficult to approach if a transected vertebral artery constricts and retracts into the foramen. In which case, angioembolization is more useful and effective.
In conclusion, common carotid and vertebral artery transections are associated with high stroke and mortality rates. The mainstay of treatment should be immediate and aggressive resuscitation and revascularization. Revascularization should be attempted whenever possible. Endovascular treatment, including embolization, is safe and effective when the lesion is difficult to approach. When revascularization is too difficult, ligation of the injured carotid artery can be considered as a last lifesaving resort.