Timing of Admission to the Surgical Intensive Care Unit is Associated with in-Hospital Mortality
Article information
Abstract
Purpose
The relationship between the timing of admission (work-hours or after-hours) to the intensive care unit (ICU) and mortality among surgical ICU (SICU) patients is unclear. This study aimed to investigate whether admission to SICU during after-hours was associated with in-hospital mortality.
Methods
This retrospective cohort study was conducted in a tertiary academic hospital. The data of 571 patients who were admitted to the SICU and whose complete medical records were available were analyzed. Work-hours were defined as 07:00 to 19:00 Monday to Friday, during which the ICU was staffed with intensivists. After-hours were defined as any other time during which the SICU was not staffed with intensivists. The primary outcome measure was in-hospital mortality according to the time of admission (work-hours or after-hours) to the SICU.
Results
A total of 333 patients, were admitted to the SICU during work-hours, and 238 patients after-hours. Unplanned admissions (47.1% vs. 33.3%, p < 0.001), acute physiology and chronic health evaluation II score ≥ 25 (23.9% vs. 11.1%, p < 0.001), the need for ventilator support (34.0% vs. 17.4%, p < 0.001), and the use of vasopressors (50.0% vs. 33.3%, p < 0.001) were significantly higher in the after-hours group compared with the work-hours group. Multivariate analyses revealed that the timing of SICU admission was an independent predictor of in-hospital mortality (odds ratio, 2.526; 95% confidence interval, 1.010–6.320; p = 0.048).
Conclusion
This study showed that admission to the SICU during after-hours was associated with increased in-hospital mortality.
Introduction
Adequate treatment within the first few hours after an initial insult is an important factor influencing treatment outcomes in critically ill patients [1,2]. Patients can develop a critical condition at any time, hence, critical care needs to be readily available. Previous studies have reported that higher levels of staffing with intensivists in the intensive care unit (ICU) led to significant reductions in ICU and subsequent in-hospital mortality, and in the length of hospital stay [3–8]. These improved outcomes were observed not only in the medical ICU but also in the surgical ICU (SICU) [9]. However, it might not always be possible to staff the ICU with intensivists beyond their regular working hours to cover nights and weekends because of limited resources and high costs.
Most previous studies have focused on patient outcomes related to intensivist staffing during the after-hours of medical ICUs [10–14]. The clinical outcomes in patients admitted to the SICU during the after-hours remain unclear. This study therefore aimed to evaluate whether SICU admission during the after-hours (any time when the ICU was not staffed with intensivists) was associated with higher in-hospital mortality compared with admission during work-hours.
Materials and Methods
1. Study setting and patient enrollment
This retrospective study was conducted on data from medical review charts between March 2018 and February 2019. Severance Hospital is a high-volume teaching and referral hospital in Seoul, South Korea. It has 143 ICU beds across 11 specialties. This study included surgical patients in 1 SICU and 1 mixed ICU. Severance Hospital follows a high-intensity staffing, semi-closed ICU model. The SICU is staffed from 07:00 to 19:00 from Monday to Friday by 1 intensivist with 3 years of experience and a 2nd year clinical fellow preparing for intensivist certification. A senior resident is in charge during the after-hours. Real-time consultations after-hours with intensivists are available according to the patient’s status.
Patients who were over 18 years and admitted to the SICU (for any reason) were eligible for this study. Trauma and post-transplant patients are managed directly by the surgeons in each specialty, so these patients were excluded from the study. Of the 586 patients admitted to the SICU during the study period, 571 patients with complete medical records were included in the study.
2. Data collection
Demographic data including age, sex, Acute Physiologic and Chronic Health Evaluation (APACHE) II score, admission type, cause of ICU admission, length of ICU stay, the need for ventilator support, and the use of vasopressor drugs were reviewed and analyzed. The primary outcome measure was in-hospital mortality according to the time of SICU admission (work-hours or after-hours), while the secondary outcomes measures were ICU readmission within 48 hours, duration of ventilator support, length of ICU stay, length of hospital stay, and in-hospital mortality.
3. Definitions
Work-hours were defined as 07:00 to 19:00 from Monday to Friday, during which time the SICU was staffed with intensivists. After-hours were defined as any other time during which the SICU was not staffed with intensivists. Planned admissions were defined as SICU admissions for postoperative monitoring or care after elective surgery, while all other admissions were defined as unplanned admissions. Patients who underwent emergency operations and developed postoperative sepsis, bleeding, or other medical complications were defined as patients with unplanned admissions. ICU readmission within 48 hours was defined as admission to the ICU within 48 hours of leaving the ICU.
4. Statistical analysis
Between-group differences were evaluated using the chi-square test or Fisher’s exact test. Continuous variables were compared using the student t test. The Cox proportional hazards model was used for the multivariate analysis. All statistical tests were 2-sided, and a p < 0.05, was considered statistically significant. All statistical tests were performed using SPSS Version 25.0 (IBM, Armonk, NY, USA).
Results
1. Clinicodemographic characteristics
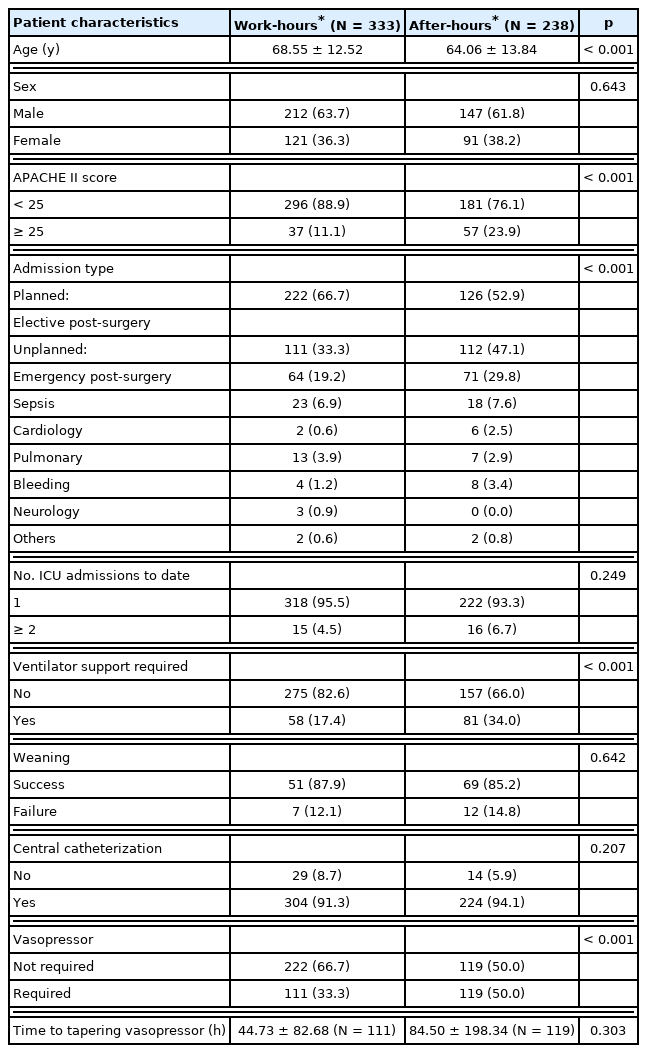
A total of 333 (58.3%) and 238 (41.7%) patients were admitted to the SICU during work-hours, and after-hours, respectively. The patients in the work-hours group were significantly older than those in the after-hours group. The number of patients with an APACHE II score of ≥ 25 was 2 times higher in the after-hours group compared with the work-hours group (23.9% vs. 11.1%, p < 0.001). Moreover, the proportion of patients with unplanned admissions, ventilator support, and vasopressor administration was also higher in the after-hours group (Table 1).
2. Comparison of clinical outcomes between groups
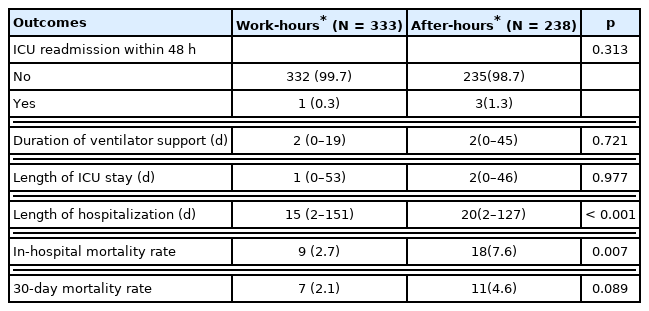
The rate of ICU readmission within 48 hours was not significantly different between the 2 groups (1.3% vs. 0.3%, p = 0.313). The median length of hospital stay was 20, and 15 days in the after-hours, and work-hours groups, respectively (p < 0.001). The in-hospital mortality rate was approximately 3 times higher in the after-hours group compared with the work-hours group (7.6% vs. 2.7%, p = 0.007; Table 2).
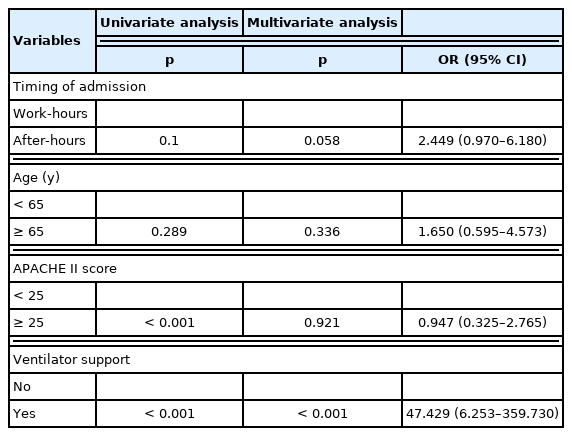
3. Univariate and Multivariate logistic regression analysis for in-hospital mortality
Multivariate analyses showed that the time of SICU admission (work-hours or after-hours) was an independent risk factor for in-hospital mortality [odds ratio (OR), 2.526; 95% confidence interval (CI), 1.010–6.320; p = 0.048]. Unplanned admission (OR, 21.607; 95% CI, 2.789–167.407; p = 0.003), and ventilator support (OR, 52.269; 95% CI, 6.920–394.808; p < 0.001) were also clinically significant independent predictors of in-hospital mortality (Table 3).
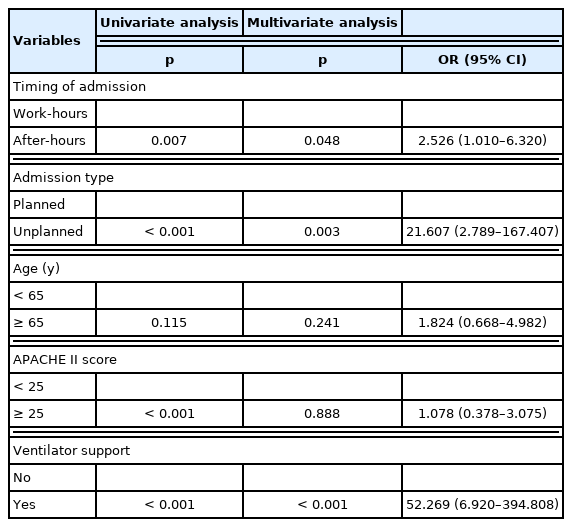
Univariate and multivariate logistic regression models for factors associated with in-hospital mortality.
4. Subgroup analysis in the planned and unplanned admission cohort
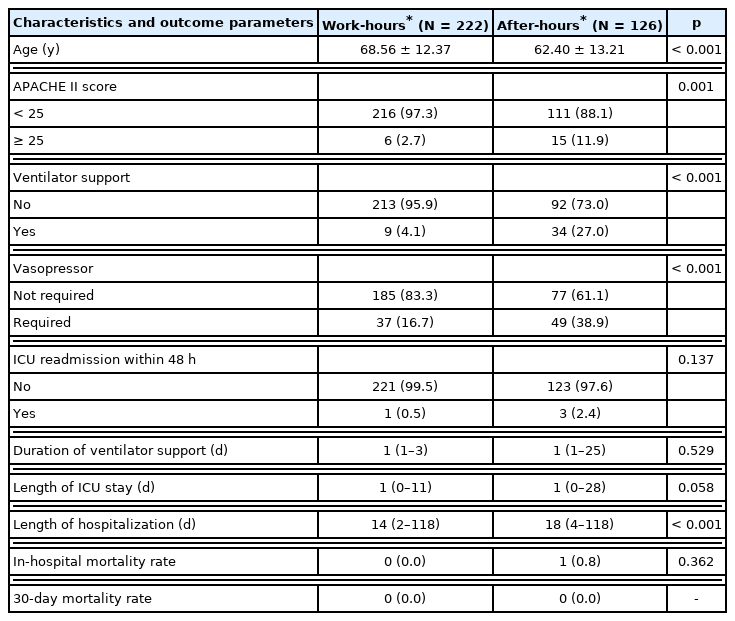
The planned, and unplanned admission subgroups comprised 348, and 223 patients, respectively. The proportion of patients with ventilator support or who required vasopressors was also higher in the after-hours group compared with the work-hours group (27.0% vs. 4.1%, p < 0.001; 38.9% vs. 16.7%, p < 0.001). The median length of hospital stay was significantly longer in the after-hours group compared with the work-hours group (18 days vs. 14 days, p < 0.001). Only 1 patient died (in-hospital mortality: 0.28%) in the planned admission subgroup.
There were 26 patients who died in the unplanned admission subgroup (in-hospital mortality 10.31%). There was no significant difference between the after-hours and work-hours groups in terms of the median length of hospitalization (20 days vs. 18 days, p = 0.977), and in-hospital mortality (15.2% vs. 8.1%, p = 0.100) in the unplanned admission subgroup (Table 5). In multivariate analysis, the time of SICU admission (work-hours or after-hours) was not associated with increased in-hospital mortality in the unplanned admission subgroup (OR: 2.449; 95% CI: 0.970–6.180; p = 0.058; Table 6).
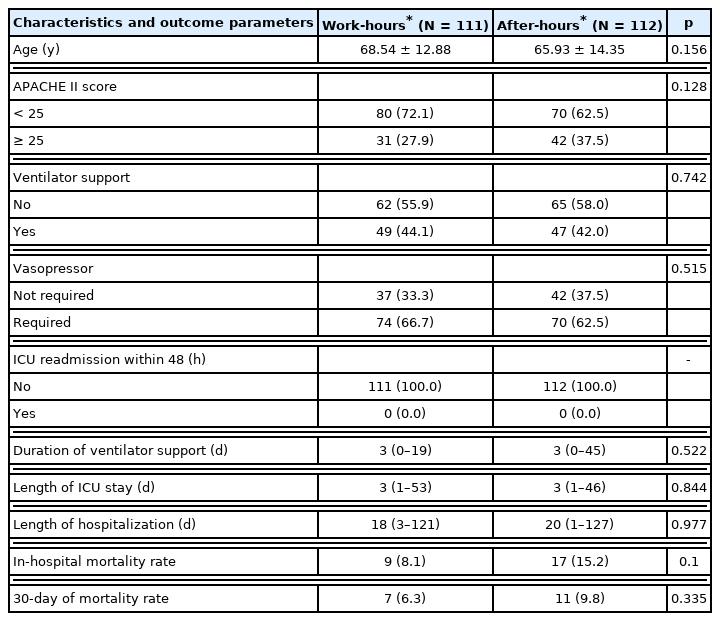
Clinicodemographic characteristics and outcomes according to the time of admission in the 223 patients who had unplanned SICU admissions.
Discussion
Previous studies have shown that the level of intensivist staffing in the ICU leads to a significant reduction in mortality and length of hospital stay [3–9]. However, the Society of Critical Care Medicine guidelines do not recommend 24/7 intensivist staffing in the ICU in high-intensity ICU models [5] based only on a randomized cohort study conducted in a medical ICU [15]. To date, there is a lack of evidence regarding the safety of admission to the SICU during after-hours.
This study investigated whether SICU admission during after-hours was associated with in-hospital mortality compared with admission during work-hours. It was determined that admission to the SICU during the after-hours period increased in-hospital mortality. Moreover, unplanned admissions, APACHE II score ≥ 25, the need for ventilator support, and the administration of vasopressor drugs were also markedly higher in the after-hours group compared with the work-hours group. These findings are important for the allocation and distribution of ICU resources, including intensivists.
According to 2 systematic reviews, while patients admitted to an ICU over the weekend were at a higher risk of dying, admission to the ICU overnight did not appear to be associated with increased mortality [16,17]. The authors inferred that low levels of staffing and intensity of care provided by many hospitals over the weekend might account for this finding [5,16,17]. In this current study, “after-hours” was defined as the absence of intensivists, and the results showed increased mortality in patients admitted to the SICU. Although there was no change in the level of nursing staff, intensity of care, and intensivists available for real-time consultations, the absence of an intensivist on the SICU may affect resolute decisions which are required during the care of patients with a critical illness.
A recent study reported that ICU admission after elective surgery during the after-hours was associated with significantly higher rates of postoperative complications, increased length of hospital stays, and increased inter-hospital transfers [18]. In this current study, the subgroup analysis of patients admitted for planned surgery showed a significantly higher severity of illness as measured by the APACHE II score, and use of ventilator or vasopressors in the after-hours group compared with the work-hours group. The length of hospitalization in the after-hours group was significantly higher than the work-hours group (work-hours vs. after-hours = 14 days vs. 18 days, p < 0.001). Further analysis was performed on the estimated blood loss and duration of the operation in this subgroup. In the after-hours group, the patients with planned admissions experienced more blood loss (work-hours vs. after-hours = 417.72 ± 647.09 minutes vs. 1,026.98 ± 1,503.99 minutes, p < 0.001) and longer operation times (work-hours vs. after-hours = 298.56 ± 160.58 minutes vs. 500.20 ± 212.18 minutes, p < 0.001, data not shown). This result suggests that cases with unexpected events during the operation are referred to the SICU after-hours, and this has an effect on the status of the patients’ severity of illness.
Even though admission after-hours showed increased in-hospital mortality in the entire cohort, other predictors,
Despite the retrospective design and short study period of this investigation, the findings may reflect the current status of most ICUs in South Korea, considering that 82.3% of all ICUs are either university teaching hospitals or university-affiliated hospitals [19]. One of the main strengths of this study was that surgical patients were specifically targeted. Recently, Kyu et al [20] conducted a retrospective observational study of 10,708 postoperative patients and reported an increased risk of 30-day mortality in the group without intensivist cover. Compared to previous studies which were performed in mixed or medical ICUs [12,14,21–28], this study only focused on postoperative SICU admissions. This study included patients with unplanned admission, including those who underwent emergency operations and those who developed postoperative sepsis, bleeding, or other medical complications, as well as those who had an elective postoperative status. Thus, the patients in this study represented the general population of patients who required postoperative intensive care, and the results were consistent with those of previous studies [18,20,29]. Additionally, subgroup analyses was performed according to the causes of SICU admission to adjust for the negative effects of unplanned admission on mortality.
In conclusion, admission to the SICU during the after-hours was associated with increased in-hospital mortality. These findings may provide a guide to hospitals for improved patient safety and the allocation of ICU resources. Staffing with 24/7 intensivist is considered ideal, but it should be operated flexibly according to each hospital’s human and material resources.
Notes
Author Contributions
MKK: Data acquisition, formal analysis, methodology, original draft, reviewing and editing. EJJ and SKP: Conceptualization, supervision, reviewing and editing. IK Kim: Conceptualization, methodology, supervision, original draft, reviewing and editing.
Conflicts of Interest
There is no conflicts of intester to declare.
Ethical Statement
This study was approved by the institutional review board of Severance Hospital, Yonsei University College of Medicine, Korea (no.: 4-2019-0412). The requirement for informed consent was waived because of the retrospective nature of the study
Data Availability
All relevant data are included in this manuscript.
Funding
The authors received no financial support for the research, authorship, and/publication of this article.