To Reduce the Incidence of Postoperative Intraabdominal Abscess, the Application of Nonoperative Management Should be Circumspect Considering Patient Factors and the Nature of Acute Appendicitis
Article information
Abstract
Purpose
Surgery and nonoperative management (NOM) are the treatment modalities for acute appendicitis (AA). There is little evidence to indicate which treatment method should be performed according to the patient's condition or disease severity, surgical extension, and timing after an appendectomy. This study aimed to evaluate postoperative intra-abdominal abscess (PIAA) associated with these factors.
Methods
The medical records of 839 patients who underwent appendectomy after a diagnosis of AA between 2019 and 2020 at Gangneung Asan Medical Centre were reviewed retrospectively. The factors associated with PIAA were evaluated.
Results
Postoperative complications occurred in 92 patients. Following appendectomy, 16 (1.9%), 83 (9.9%), and three (0.4%) patients developed PIAA, surgical site infection, and incisional hernia, respectively. The American Society of Anesthesiologists class, complicated appendicitis on preoperative abdominal computed tomography, failure of NOM, and extensive surgery above appendectomy were associated with the development of PIAA. However, a laparoscopic approach, irrigation, indwelling drain, ultrasonic dissection, and use of sterile bags were not associated with the development of PIAA.
Conclusion
NOM for some patients with complicated AA is an attractive treatment modality. However, to reduce the incidence of PIAA, the application of NOM should be circumspect considering patient factors and the nature of acute appendicitis. Furthermore, appendectomy should be performed as early as possible for patients not indicated for NOM.
Introduction
Acute appendicitis (AA) may develop due to obstruction of the appendix orifice [1]. Bacterial overgrowth and mucus secretion increases the intraluminal pressure and diameter of the appendix. Patients with early phase appendicitis complain of periumbilical visceral pain owing to intraluminal distention of the appendix. Furthermore, ischemic injury progresses with impairment of lymphatic and venous drainage. These complicated processes lead to gangrene, perforation, and abscess formation due to localized inflammation. Advanced localized inflammation incurs right lower abdominal pain caused by the irritation of the peritoneum around the appendix [2].
The treatment of appendicitis varies according to the patient’s condition and disease severity [3,4] Several retrospective studies and randomized clinical trials have investigated nonoperative management (NOM) such as intravenous antibiotics (IV anti), and percutaneous catheter drainage (PCD), and reported the effects of NOM are similar to those of surgery [5–7]. NOM has several benefits such as reduction of operational risks in high-risk patients [8]. Furthermore, NOM may result in less pain, complications, and anxiety. However, some surgeons favor traditional appendectomy for several reasons. Firstly, a complete recovery is anticipated. Secondly, nonoperative interventions have greater medical costs and a longer therapeutic period than surgery. Thirdly, the anatomy of the appendix is not complex, and an appendectomy is a relatively simple procedure with a high success rate [9]. Although AA is a benign condition/disease and the level of difficulty of surgery is low, in some cases, an appendectomy is challenging for surgeons because of various treatment modalities, and postoperative complications [10].
An appendectomy is one of the most common emergency operations in the Department of General Surgery [11]. An uncomplicated appendectomy primarily requires the correct use of the surgical instruments and basic knowledge of abdominal anatomy. Hence, the learning curve for appendectomy is short [12]. Furthermore, the development of surgical instruments and skills has facilitated appendectomy. However, appendectomies for some cases of complicated appendicitis are difficult. Depending on the patient’s general condition, degree of appendicitis, timing until surgery, and surgical technique, the extent of surgery and incidence of complications may vary. The treatment guidelines for AA were published several years ago [13]. However, there are no definite criteria for the selection of treatment method and timing until surgery according to the patient condition and disease severity. Hence, many surgeons depend on their experience due to the lack of evidence for appendicitis treatment decision making [14].
Therefore, this study primarily aimed to evaluate the incidence of postoperative complications associated with a patient’s general condition, disease severity, and surgical timing. The secondary aim was the evaluation of clinical variables associated with postoperative intra-abdominal abscess (PIAA).
Materials and Methods
1. Study design
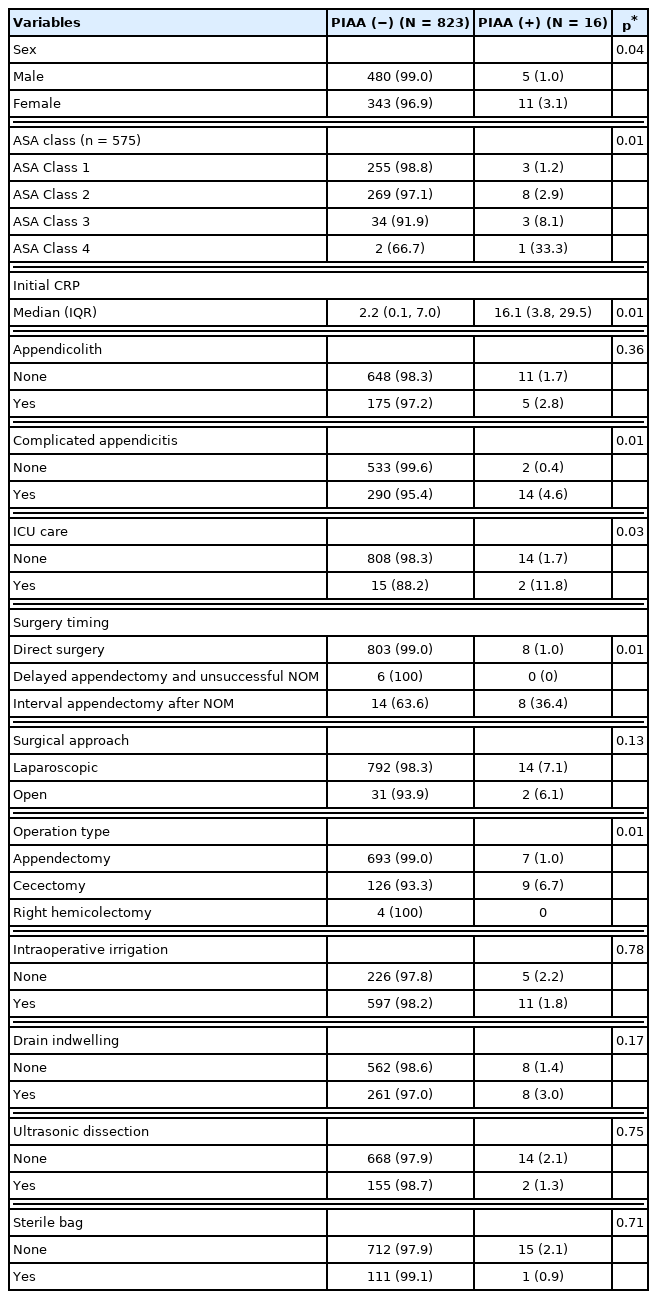
This retrospective study was performed using medical data collected from Gangneung Asan medical center, a tertiary hospital in Gangneung, Republic of Korea. The study included patients diagnosed with AA who underwent appendectomy between January 2019 and December 2020. Patient data were obtained from electronic medical records. Patients whose data was missing (N = 4) and those who underwent nonoperative intervention (N = 12) were excluded. This study was approved by the Institutional Review Board of the Gangneung Asan Medical Centre (no.: 2021-08-014). The requirement for written informed consent was waived owing to the retrospective nature of the study.
2. Treatment protocol
Patients who complained of abdominal pain or were diagnosed with AA at community hospitals were initially examined by a physician in the Department of Emergency Medicine. The physician collected data on physical examination findings and laboratory values of patients suspected of having AA. All patients suspected of having AA underwent contrast or non-contrast abdominal computed tomography (ABD CT) at Gangneung Asan Medical Center. ABD CT data were analyzed by three abdominal radiologists who determined the diameter and thickness of the appendix, wall enhancement, wall defect, and peri appendiceal haziness. Suspicion of an extraluminal appendicolith, appendix perforation with a defect in the enhancing appendiceal wall, and abscess or phlegmon based on ABD CT was defined as complicated appendicitis. The treatment strategy was planned based on the surgeon’s preferences and considering patient’s vital signs, general condition, nature of appendicitis, and availability of the operating room. Treatment for appendicitis included direct surgery or NOM followed by interval surgery (Figure 1). Regarding the timing of surgery, direct surgery was performed within one day of admission, interval appendectomy was performed four weeks after diagnosis, and delayed appendectomy was performed between 3 days to 4 weeks due to unexpected aggravation of appendicitis. Nine surgeons performed appendectomies during the study period. Four pathologists defined AA as the infiltration of neutrophils into the mucosa. Postoperative complications were defined as any deviation from the normal postoperative course. Surgical site infection was defined as an infection at the incision site, and PIAA was defined as an infection that develops at the appendiceal stump as a direct result of the appendectomy.
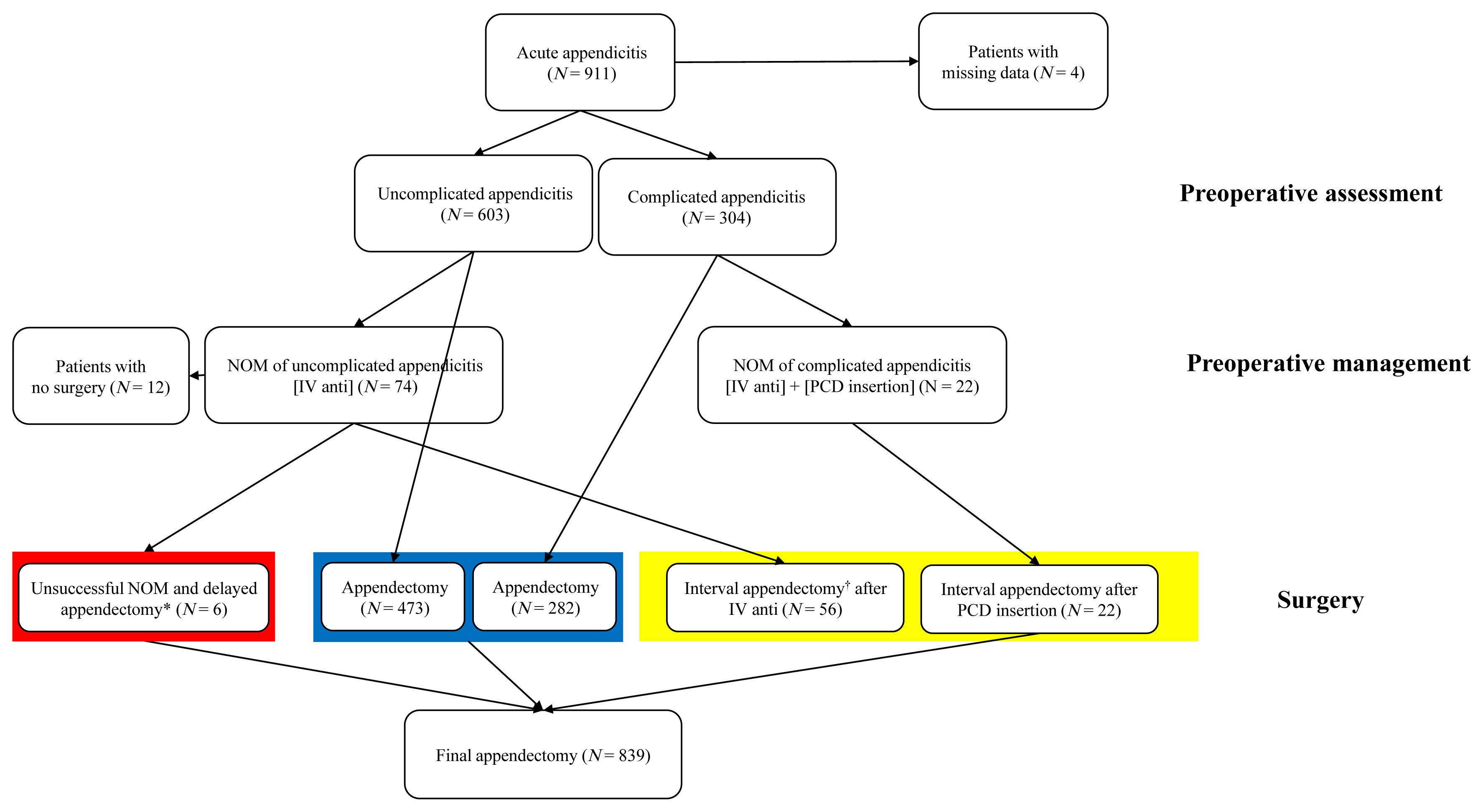
Flowchart of included patients.
* Delayed appendectomy: Appendectomy performed between 24 hours and one week after diagnosis.
† Interval appendectomy: Elective appendectomy performed at least four weeks after NOM.
NOM = nonoperative management; IV anti = intravenous antibiotics; PCD = percutaneous catheter drainage.
3. Data and statistical analysis
Data was collected on the following: age, sex, height, weight, past medical history, medication history, and American Society of Anesthesiologists (ASA) Physical Status Classification System class which predicted a patient’s preanesthesia medical comorbidity [15]. Furthermore, image findings, timing before surgery, method of surgery, and complications were extracted from medical records. The complications after appendectomy were analyzed. Subsequently, all patient data were divided into the PIAA and non-PIAA groups. Clinicopathological and treatment variables were compared between the groups using the Mann-Whitney U test for non-normally distributed quantitative variables and the Chi-square test or the Fisher’s exact test for categorical data analysis. Multivariate analysis was performed using a binary logistic regression model to identify predictive factors of PIAA after the 1st treatment. Significant variables in univariate analysis were included in multivariate analysis as confounding variables. All statistical analyses were two sided, and a p < 0.05 was considered statistically significant. Statistical analyses were performed using IBM SPSS Version 23.0 (Armonk, NY, USA).
Results
1. Patient characteristics
A total of 839 appendectomies were performed between 2019 and 2020 at Gangneung Asan Medical Centre. The characteristics of patients with AA are presented in Table 1. The median age of patients was 44 years [159 (19.0%) patients: < 20 years; 158 (18.8%) patients: > 65 years; and 522 (62.2%) patients: 20–64 years]. The medical and medication histories of patients were assessed for the presence of hypertension and diabetes mellitus. The ASA Physical Status Classification System class revealed that 30 patients were classified with severe systemic disease. Seventeen patients with septic shock or an underlying disease were admitted to the intensive care unit (ICU) during the perioperative and postoperative period.
2. Appendicitis nature
The appendicitis-related characteristics are shown in Table 1. The median duration of illness before arrival at the hospital was 27 hours. The median concentration of initial C-reactive protein (CRP) was 2.3 mg/dL. A total of 180 patients were diagnosed with AA and appendicolith, and 304 patients were diagnosed with complicated appendicitis based on preoperative ABD CT. Complicated appendicitis positively correlated with the duration of illness before presentation to the hospital and measurement of the initial CRP concentration (Pearson correlation coefficient: 0.216, p = 0.01 and Pearson correlation coefficient: 0.352, p = 0.01, respectively).
3. Appendectomy
A total of 78 patients underwent interval surgeries, including uncomplicated and complicated appendicitis with NOM (IV anti ± PCD insertion) completion. Delayed appendectomies were performed on six patients due to failure to the NOM or delayed diagnosis. Most patients (91.1%) underwent laparoscopic appendectomy. A total of 139 (16.6%) patients underwent cecectomy. Intraoperative irrigation, drain placement, use of the sterile bag, and ultrasonic dissection were performed based on surgeon preference and access to the intraoperative surgical field. Negative appendicitis (normal appendix) was confirmed in 31 patients. The positive predictive value of ABD CT for appendicitis was 0.963.
4. Postoperative complications
Postoperative complications occurred in 92 patients (102 cases; Table 1). A total of 29 and 38 cases were included in Clavien-Dindo classification category 3 and 2, respectively. None of the patients died. Sixteen patients developed PIAA (Figure 2). Seven patients required PCD insertion, eight patients required a prolonged hospital stay, and one patient required reoperation. The results of subgroup analysis of PIAA-related characteristics are presented in Table 2. The incidence of PIAA increased with the increase in ASA class. Complicated appendicitis and preoperative ICU care were related to PIAA. None of the patients who underwent interval appendectomy developed PIAA after PCD insertion. However, 67.8% patients who underwent delayed appendectomy because of appendicitis aggravation, despite IV anti, developed PIAA. Compared with appendectomy, extended surgery was associated with the development of PIAA. No statistical difference was detected between the groups in terms of the surgical approach; intraoperative irrigation; and use of ultrasonic dissection, a sterile bag, and a drain. Several variables were significantly associated with PIAA in univariate analysis (Table 3). Treatment-related variables, such as timing until surgery and extent of surgery, and patients’ clinical factors, such as sex, ASA class, initial CRP level, preoperative ICU care, and nature of appendicitis, were associated with the development of PIAA.
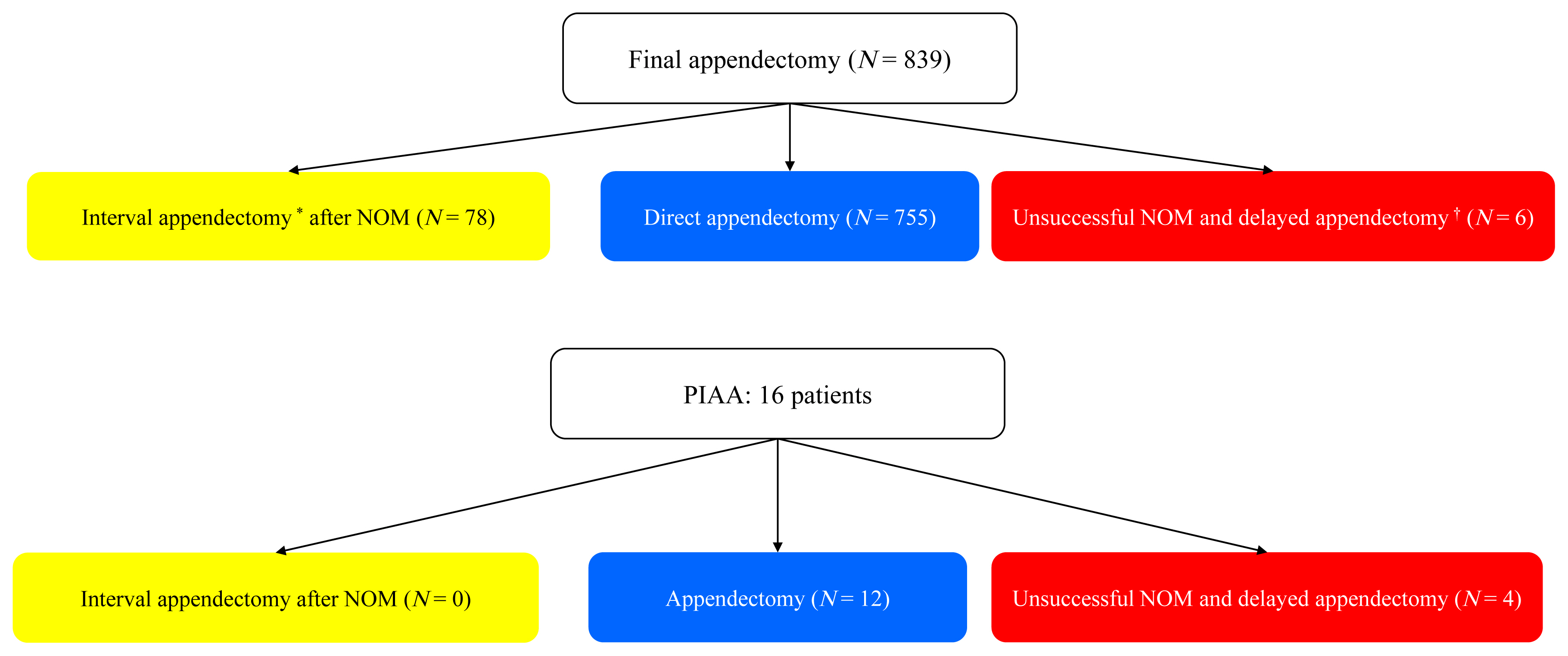
Number of patients with postoperative intra-abdominal abscess according to surgical timing.
* Delayed appendectomy: Appendectomy performed between 24 hours and one week after diagnosis.
† Interval appendectomy: Elective appendectomy performed at least four weeks after NOM.
NOM = nonoperative management; PIAA = postoperative intra-abdominal abscess.
Discussion
This study determined the rate of PIAA after appendectomy considering comorbidity, nature of the disease progression, and method or timing until surgery. Mostly, AA develops owing to a closed-loop obstruction when the orifice is blocked due to the small orifice and long body structure. The therapeutic approach for AA is challenging because of various treatment modalities, patient factors, and disease severity. A surgeon’s experience has a great influence on treatment decision making for treatment of AA because no definite criteria are available. Hence, to reduce complications, the reporting of postoperative complications in patients with AA who have undergone surgical procedures is necessary.
Traditionally, untreated simple AA might progress to complicated appendicitis based on the natural course. Therefore, to prevent perforation or peritonitis when the diagnosis is ambiguous, an emergency appendectomy is performed for rapid treatment. However, a previous study suggested that simple and complicated appendicitis have different etiologies on progression [16]. Yeh et al [16] suggested that some cases of simple appendicitis did not progress to complex appendicitis without treatment. Furthermore, it is challenging to prevent perforation with rapid treatment because most cases of complex appendicitis occur before arrival at the hospital. These results do not indicate that all cases of appendicitis do not require surgery. Hence, distinguishing patients with appendicitis who require surgical treatment from those who can recover with NOM is necessary [17]. Patients who require surgical treatment have a poor prognosis and develop complications if surgery is delayed.
In the current study, a correlation between the duration of abdominal pain before arrival at the hospital and occurrence of appendix perforation was observed. Gangneung Asan Medical Center is the only tertiary hospital in the region, and the proportion of patients who require surgical treatment is high and the proportion of patients who self-recover is low. The progression of appendicitis might be closely related to the natural course of appendicitis and the underlying systemic disease in patients [17]. The incidence of complications was high in patients with a high ASA class and complicated appendicitis at the time of surgery. It appears that each patient responds differently depending on the individual underlying condition/disease. The current state of appendicitis and systemic disease of the patient should be considered during decision making regarding surgery for appendicitis.
In the current study, all patients with AA underwent ABD CT. The rate of negative appendectomy was only 3%. Although there may be concerns regarding radiation exposure and increased medical expenses, the diagnostic performance of ABD CT is higher than the scoring system that combines symptoms, physical examination, and laboratory findings. ABD CT is not an absolute standard, but it is a tool for diagnosis and treatment decision making which considers symptoms, physical examination, and blood test findings. A previous study has elucidated the limitations of ABD CT for predicting the severity of appendicitis [18]. However, it is feasible to overcome this limitation through the analysis of specific image findings by an experienced radiologist [19]. The etiology of AA can be deduced from the presence of appendicoliths. Furthermore, the current state of the appendix can be inferred from specific imaging findings such as phlegmon, abscess, intraperitoneal or periappendiceal fluid collection, and mucosal hyperenhancement. This preoperative imaging provides important clues for the diagnosis of appendicitis and determining the treatment direction and timing [20].
All cases of delayed surgery originated from unsuccessful NOM. Delayed surgery was associated with an increased incidence of intra-abdominal abscess. Patients with complicated appendicitis at the time of arrival at the hospital had a high rate of PIAA compared with uncomplicated appendicitis. Additionally, the course of complicated appendicitis and untreated appendicitis are considered to be similar. The traditional pathophysiology of AA can be applied to patients who require surgical treatment. It has been reported that open surgery increased the incidence of surgical site inflammation [21]. However, our data did not reveal any such findings, although our study only included 33 cases of open surgery. In addition, the relationship between the use of sterile bags, intraperitoneal irrigation, drain placement, and the use of ultrasonic dissection and PIAA has been investigated [19]. In the current study, the surgical method was not significantly related to the occurrence of PIAA. However, if surgery was delayed or extended in patients who required surgery, the rate of PIAA increased. Hence, treatment decision making should be performed. If surgery is required, the appropriate time before surgery and method of surgery should be determined by comprehensively considering the systemic condition and status of appendicitis.
This study has several limitations. This was a single-center retrospective study with a study population that included many patients who were referred for surgical treatment after diagnosis in other hospitals. Additionally, the study included only patients who had undergone surgery; therefore, selection bias may exist. It is difficult to examine the natural course of appendicitis in a study on the occurrence of PIAA after surgery and whether it can indicate surgery.
Conclusion
We analyzed the incidence of PIAA, which increases the medical cost and the length of the hospital stay. The patient’s general condition, severity of the disease, and extent and timing prior to surgery are related to the development of PIAA after appendectomy. To reduce the incidence of PIAA, the application for NOM should be studied and decision making for AA should be performed as early as possible, considering the general condition of patients and severity of the disease.
Acknowledgments
This study was presented at the Annual Congress of the Korean Surgical Society in Seoul, Korea, in November 2021. The authors are grateful to all participants.
Notes
Conflicts of Interest
The authors declare that they have no competing interests.
Author contributions
Resources, Investigation, Formal analysis, Writing - Original Draft: YJL. Conceptualization, Methodology, Validation, Supervision: KHY.
Ethical Statement
This research did not involve any human or animal experiments.
Data Availability
All relevant data are included in this manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.