|
 |
- Search
| J Acute Care Surg > Volume 12(3); 2022 > Article |
|
This article has been corrected. See J Acute Care Surg. 2023 Jul 24; 13(2): 83.
Abstract
Pancreatic injury is rare in pediatric cases of blunt abdominal trauma and nonoperative management is preferred in pediatric patients. There are more concerns about operative treatment observed in pediatric patients compared with adult patients. However, some pediatric cases require surgical treatment. If distal pancreatectomy is performed, the necessity of splenectomy should be considered, especially in pediatric patients. This study reports the case of a 17-month-old patient with a Grade 3 pancreatic injury following blunt abdominal trauma. The patient was successfully managed by spleen-preserving distal pancreatectomy. In conclusion, this surgical technique can be performed safely, and complications caused by splenectomy can be prevented using this technique.
In pediatric cases of blunt abdominal trauma, the pancreas is the 4th most common solid organ that is affected [1]. When comparing patients who have sustained trauma, pancreatic injury is less common in the pediatric patients compared with adult patients, and principles for treatment have not yet been established. In addition, more concerns about operative treatment are observed in pediatric patients and nonoperative management (NOM) is considered first [2]. In cases where operative treatment is unavoidable, it may be considered depending on the grade of the injury. Distal pancreatectomy is mainly performed when pancreatic resection is required. Thus, it is important to consider whether a splenectomy is necessary. Although the spleen is often resected via distal pancreatectomy in adults, the approach is different in pediatric patients. Thus, the functions of the spleen, such as immunity, should be considered. Recently, spleen-preserving distal pancreatectomy has been performed in patients with trauma and general pancreatic disease [3]. Herein, we present a case of spleen-preserving distal pancreatectomy in a pediatric patient with pancreatic injury.
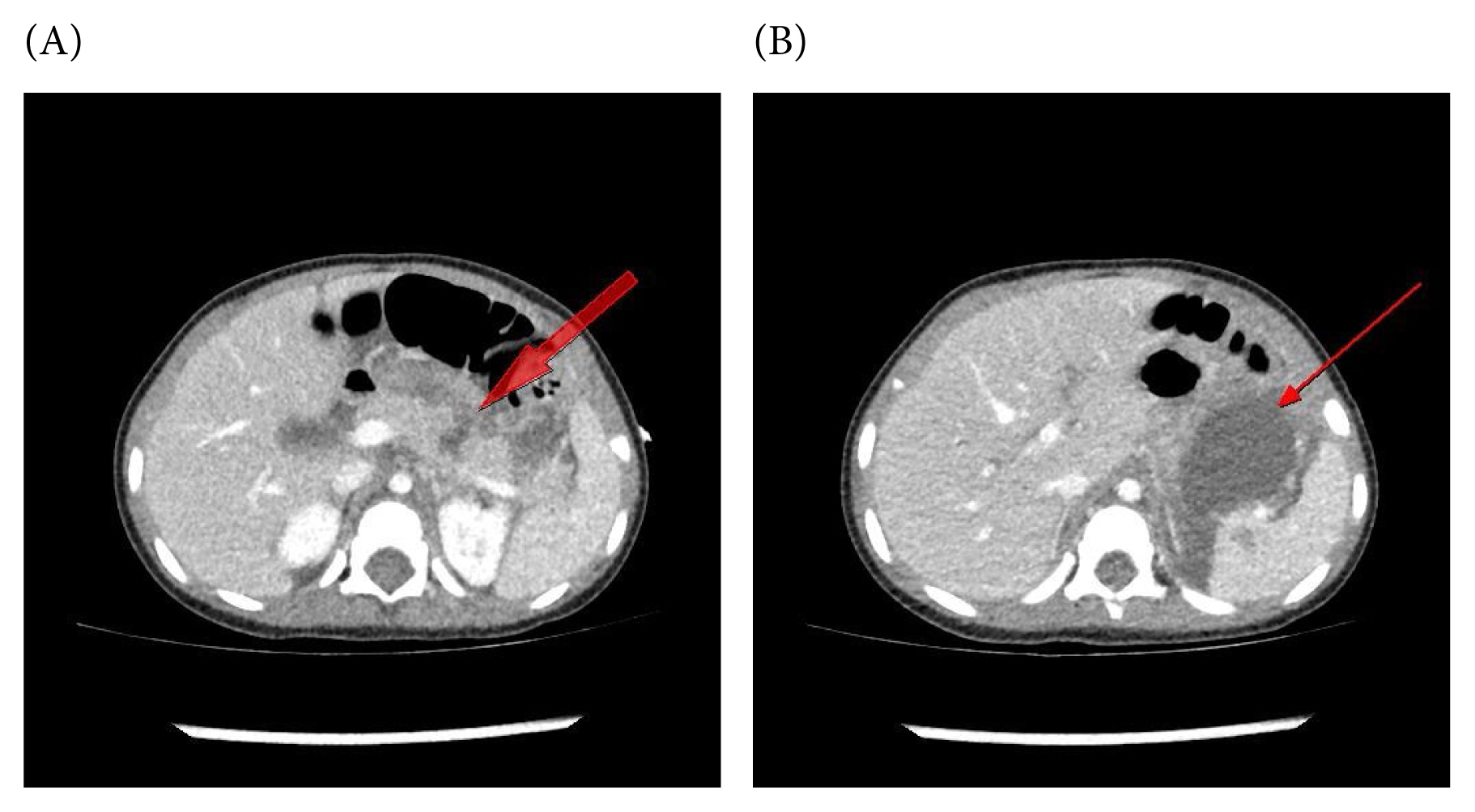
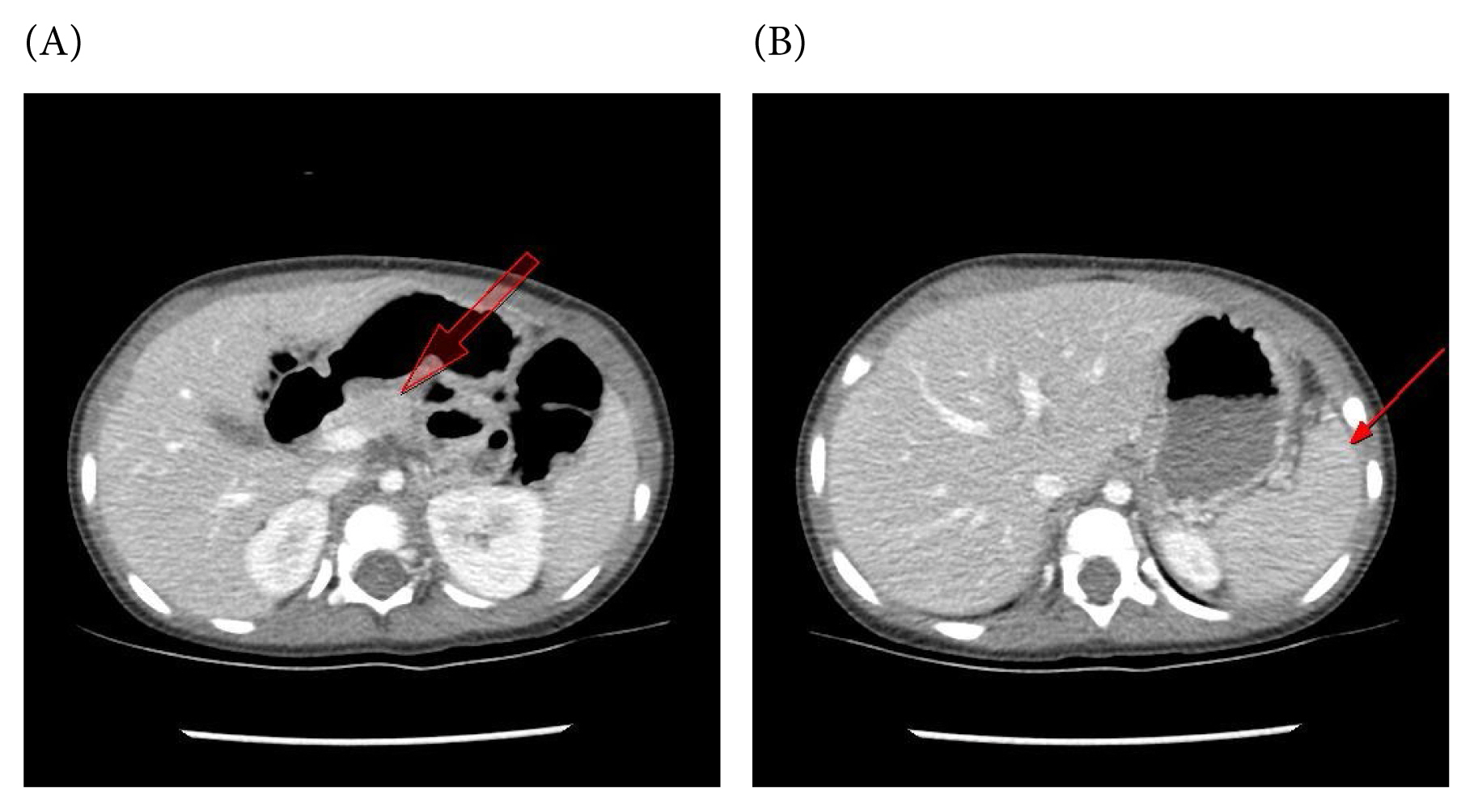
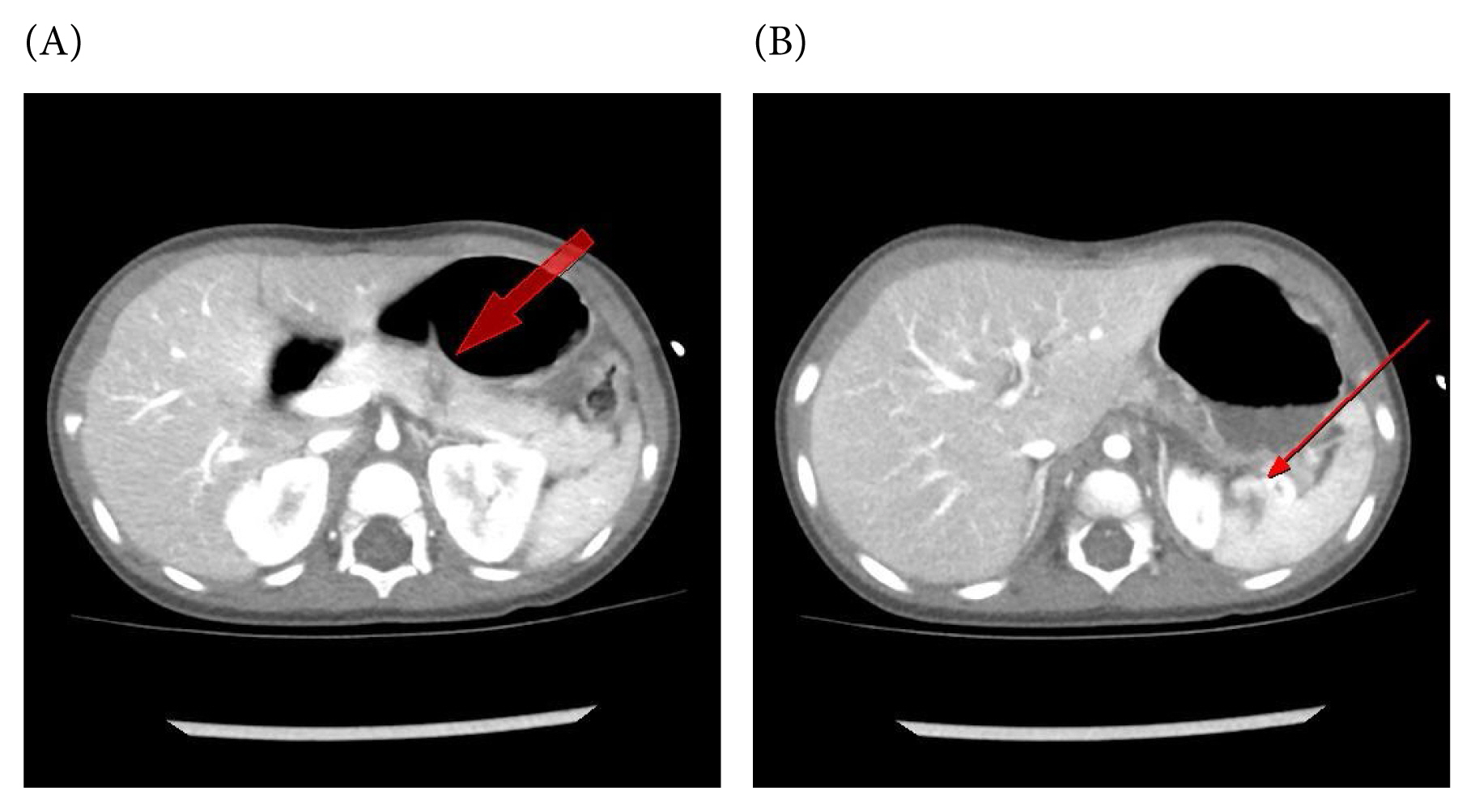
A 17-month-old girl was transferred to a trauma center following a traffic accident. At the time of admission, she weighed 13kg and her blood pressure were normal; however, she had tachycardia. Moreover, she exhibited a stuporous mental status and was transferred to our hospital after undergoing endotracheal intubation at another hospital. Her vital signs were stabilized after resuscitation, and evaluations, such as computed tomography (CT) were performed. Contrast-enhanced abdominal CT revealed pancreatic body fracture with minor spleen injury (Figures 1A and 1B). Concomitant injuries included a large scalp degloving injury and lung contusion. Considering her young age and stable vital signs, another CT was performed after 2 days, and the necessity of surgery was deliberated. Follow-up abdominal CT revealed increased intra-abdominal fluid collection (Figures 2A and 2B); moreover, she developed fever. Thus, surgery was performed. Although spleen injury was observed, active bleeding from spleen was not clear, and considering the patientŌĆÖs age, a spleen-preserving distal pancreatectomy was performed. Intraoperatively, the pancreas was dissected from the surrounding tissues using an energy device (LigaSure), and was excised using a scalpel proximal to the injured site. After confirming main pancreatic duct, the duct and pancreatic stump were sutured, respectively. A drain was placed around the stump. The splenic artery and vein were ligated, and short gastric arteries were preserved. Splenic circulation was confirmed based on color, and the spleen was preserved. The duration of operation was 3 hours. After her consciousness improved, extubation was performed on Day 2 post surgery. Oral feeding was initiated on Day 5, and the drains were removed on Day 10 following surgery. Due to concomitant injuries, the patient was discharged without any complications, such as bleeding or major pancreatic fistula, after 1 month. On follow-up CT performed at 3 months, the spleen was well preserved without abnormal findings (Figures 3A and 3B).
Pancreatic injury following blunt abdominal trauma is uncommon in pediatric patients. The incidence of pancreatic injury in pediatric cases of blunt abdominal trauma ranges from 3% to 12% [1]. Early diagnosis and treatment are important to reduce morbidity and mortality. Pedestrian accidents are the most common cause of pancreatic injury in children [4]. If abdominal trauma is suspected, the possibility of pancreatic injury should be considered. In particular, lumbar spine injury is often accompanied by pancreatic injury [5].
Ultrasonography plays an important role in the initial evaluation of patients with trauma. However, diagnosis via ultrasonography is difficult because the pancreas is a retroperitoneal organ. Hence, CT is important for diagnosing pancreatic injury. Moreover, abdominal CT is useful for identifying injuries to abdominal organs other than the pancreas. Thus, it is the preferred imaging modality for patients with abdominal trauma. However, it should be performed only when the patientŌĆÖs vital signs are stable. Magnetic resonance cholangiopancreatography may also be helpful, but it can be limited in the early stages of multiple traumas. Endoscopic retrograde cholangiopancreatography (ERCP) can help in the diagnosis and treatment of pancreatic injury and plays an important role in NOM. ERCP can be performed safely, even in children [6]. However, in reality, only a few hospitals can perform ERCP in pediatric patients. Although the trauma center in this study is a tertiary general hospital, pediatric ERCP is rarely performed because of the lack of experienced medical staff and resources. Moreover, performing the procedure is particularly difficult in infants and toddlers. Furthermore, ERCP is often limited by unstable vital signs, multiple traumas, or the use of a mechanical ventilator.
Pancreatic injuries are graded and treatment methods vary depending on the location or degree of injuries. In adult patients with Grade 1 or 2 minor pancreatic injury NOM is preferred, whereas operative management is performed in those adult patients with Grade 3 or higher pancreatic injury [7]. In pediatric patients, operative management is a concern, and a previous study showed that NOM is possible even in pediatric patients with high grade pancreatic injuries [2].
In this current case, follow-up CT revealed increased intra-abdominal fluid collection, and the patient developed a fever. These findings suggested main pancreatic duct injury. Thus, surgical treatment was performed. As mentioned distal pancreatectomy is generally performed for Grade 3 pancreatic injury. Moreover, a laparotomy or laparoscopic surgery can be performed in these patients. Furthermore, laparoscopic surgery is usually performed in general pancreatic surgery and has recently been performed in patients with trauma, including children [8].
Regarding distal pancreatectomy, it was unclear whether the spleen should be excised or preserved. Recently, cases of spleen preservation in pancreatic surgeries [9] and reports of spleen-preserving distal pancreatectomy were reported in patients with trauma [3]. In such cases, it is important to consider post splenectomy complications such as overwhelming post splenectomy infection as well as the immune systems of children. In pediatric patients, antibiotics are recommended for several years after splenectomy [10]. If the spleen is preserved, immunity can be maintained and side effects of antibiotics may be reduced.
A spleen-preserving technique may involve preserving the main splenic artery and vein or ligating them. The method of preserving splenic vessels requires more time and is associated with the risk of postoperative bleeding. Postoperative complications such as pancreatic fistula may occur after pancreatic surgery, thereby increasing the risk of bleeding. In the present case, splenic vessels were ligated because of the presence of contusions. Even with main splenic vessel ligation, the spleen may be preserved if the short gastric vessels and left gastroepiploic vessels are preserved [11]. Thus, it is necessary to access splenic circulation based on color change in this technique.
In pediatric abdominal trauma, several factors should be considered while making decisions because some factors can cause complications and affect future growth. If possible, NOM should be considered. However, if surgery is unavoidable, spleen-preserving distal pancreatectomy can be safely performed.
Acknowledgments
This work was supported by clinical research grant from Pusan National University Hospital in 2021.
Notes
Author Contributions
Conceptualization: KGH, KSH and KJH. Methodology: KGH. Formal investigation: KGH and KSH. Data analysis: KGH and KSH. Writing original draft: KGH. Writing - review and editing: KJH and KGH.
Figure┬Ā1
Initial abdominal computed tomography: (A) Pancreatic body fracture; and (B) minor spleen injury.
References
1. Mattix KD, Tataria M, Holmes J, Kristoffersen K, Brown R, Groner J, et al. Pediatric pancreatic trauma: predictors of nonoperative management failure and associated outcomes. J Pediatr Surg 2007;42(2):340-4.


2. Garg RK, Mahajan JK. Blunt trauma pancreas in children: is non-operative management appropriate for all grades? Pediatr Gastroenterol Hepatol Nutr 2017;20(4):252-8.




3. Schellenberg M, Inaba K, Cheng V, Bardes JM, Lam L, Benjamin E, et al. Spleen-preserving distal pancreatectomy in trauma. J Trauma Acute Care Surg 2018;84(1):118-22.


4. Jobst MA, Canty TG, Lynch FP. Management of pancreatic injury in pediatric blunt abdominal trauma. J Pediatr Surg 1999;34(5):818-23. discussion 823-4.


5. Rutkoski JD, Segura BJ, Kane TD. Experience with totally laparoscopic distal pancreatectomy with splenic preservation for pediatric trauma--2 techniques. J Pediatr Surg 2011;46(3):588-93.


6. Felux J, Sturm E, Busch A, Zerabruck E, Graepler F, St├╝ker D, et al. ERCP in infants, children and adolescents is feasible and safe: results from a tertiary care center. United European Gastroenterol J 2017;5(7):1024-9.




7. Ho VP, Patel NJ, Bokhari F, Madbak FG, Hambley JE, Yon JR, et al. Management of adult pancreatic injuries: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 2017;82(1):185-99.

8. Nikfarjam M, Rosen M, Ponsky T. Early management of traumatic pancreatic transection by spleen-preserving laparoscopic distal pancreatectomy. J Pediatr Surg 2009;44(2):455-8.


9. Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra D, Conlon KC. The value of splenic preservation with distal pancreatectomy. Arch Surg 2002;137(2):164-8.