Characteristics and Risk Factors for Pressure Ulcers in Severe Trauma Patients Admitted to the Trauma Intensive Care Unit
Article information
Abstract
Purpose
A retrospective descriptive study was performed to develop strategies to manage or prevent pressure ulcers in patients with severe trauma being cared for in the trauma intensive care unit (TICU).
Methods
Study data was compiled from 315 patients with severe trauma (injury severity score ≥ 15) who were admitted to a general hospital from January 1, 2020, to February 28, 2021 and were being cared for in the TICU. For patients with pressure ulcers, the characteristics and associated factors of pressure ulcers were examined.
Results
There were 42 severe trauma patients (13.3%) with pressure ulcers, of which, 50.0% of cases occurred at the site of the coccyx. In 50% of patients, Stage 2 pressure ulcers were observed. The mean onset day of pressure ulcers was 9.74 days after admission. The occurrence of diabetes, critical care triage score, length of stay in intensive care, death, shock, dialysis, ventilator application, endotracheal intubation, peripheral insertion central catheter insertion, A-line insertion, body protector application, sedatives, blood pressure boosters, nasal cannula, high-flow oxygenators, oxygen tip application, drainage insertion, nasogastric tube nutrition, and ventilator application period were investigated. Logistic regression analysis revealed that the influencing factors for the development of pressure ulcers were endotracheal intubation, length of stay in the TICU, and age, in that order.
Conclusion
By identifying the characteristics and risk factors associated with pressure ulcers in patients with severe trauma, strategies can be developed to better prevent or manage pressure ulcers in the future.
Introduction
Trauma is defined by the World Health Organization as “harmful physical and mental health consequences that occur as a result of intentional or unintentional accidents,” and types of trauma include traffic accidents, falls, drownings, self-harm, and intentional harm [1]. Trauma is the leading cause of death worldwide, accounting for 1 in 10 deaths [2]. In the United States, unintentional injuries are the third leading cause of death among all age groups [3]. In South Korea, trauma is the leading cause of death among people under 44 years of age, and the second leading cause of death among people over 45 years of age, making trauma an important cause of death in the economically active population [4]. Recent strategies to reduce the mortality rate of trauma patients include the development of a specialized medical care system and a trauma characterization center. Regional trauma centers, originally founded in South Korea in 2012, have become established, and as of 2022, 17 centers are operating in South Korea [5].
Various indicators are used to assess the degree of trauma and predict prognosis in trauma patients. Representative tools include the Acute Physiology and Chronic Health Evaluation score, the Injury Severity Score (ISS), the Trauma Score, and the Trauma and Injury Severity Scale score. The ISS is the most widely used scoring system. It was developed in 1974 as an anatomical score measuring the severity of patients with multiple injuries. Based on the Abbreviated Injury Scale (AIS), which measures the degree of damage to the injured anatomical part by assigning a score on a six-point scale, if the sum of squares of the AIS scores from the three most severely injured parts among the six AIS anatomically injured parts (head and neck, face, chest, abdominal and internal organs in the pelvis, extremity, pelvis, and external) is ≥ 15 points, the patient is to be managed as a severe trauma patient [6].
In 2016, patients with severe trauma accounted for 18.9% of all trauma patients [7]. According to the 2016–2020 report of the Korea National Statistics Office, 100,000 cases of severe trauma per year. Patients with severe trauma have multiple fractures of the spine or limbs [8] (often associated with organ damage), and require admission to a trauma intensive care unit (TICU) after initial resuscitation at the trauma bay in regional trauma centers [7,9]. In a TICU, patients are intubated and receive mechanical ventilation, and undergo assessment according to the site of injury [9,10]. The initial stage of treatment focuses on short-term issues such as treatment for shock through damage control surgery and mass blood transfusions, medication, and changes in consciousness [11,12]. While in the long-term stage of treatment, the focus is on managing sensory integration problems and skin integrity using various therapeutic devices, rehabilitation, and return to daily activities [11,12].
Long-term restriction of movement occurs in patients with severe trauma with multiple fractures because of the use of various therapeutic devices after surgical procedures, and these patients are prone to pressure ulcers due to skin and tissue damage and poor perfusion [13]. The incidence of pressure ulcers in TICU patients outside South Korea is reported to be about 1.5 times higher than that in general ICU patients with treatment required for severe pressure ulcers [13,14]. The development of pressure ulcers is associated with prolonged ICU stay, increased morbidity and mortality, and higher medical costs [15]. TICU nurses play a key role not only in the initial treatment of severe trauma patients but also in the long-term prevention and management of pressure ulcers. Awareness of risk factors for pressure ulcers, early detection, and the implementation of preventative measures is cost-effective, and contributes to a faster recovery by avoiding unnecessary hospital stays.
International studies on severe trauma have focused on head trauma [16], chest trauma [3,13], and treatment protocols [17]. In South Korea research includes studies on nursing care in severe trauma by the site of injury [10], trauma severity classification [6], analysis of nursing intervention in patients with abdominal trauma [18], and analysis of mortality or prognosis in severe trauma cases [11]. Studies on pressure ulcers have focused on medical device-related pressure ulcers in ICU patients [19], factors contributing to the development of pressure sores in ventilated patients [20], and pressure ulcer risk assessment tools [21]. However, few studies have been conducted in South Korea investigating pressure ulcers and risk factors for the development of pressure ulcer in patients with severe trauma admitted to the TICU.
The purpose of this study was to analyze the characteristics and risk factors for pressure ulcers in severe trauma patients by using the electronic medical records of TICU inpatients in a general hospital, and provide the basic data for the implementation of preventive measures and intervention.
Materials and Methods
1. Study design
This retrospective descriptive study used secondary data analysis after extracting data from the electronic medical records of severe trauma patients admitted to the TICU, Northern Gyeonggi Trauma Center of the Catholic University of Uijeongbu Saint Mary’s Hospital.
2. Study patients
A total of 903 patients were admitted to the TICU, Northern Gyeonggi Trauma Center of the Catholic University of Uijeongbu Saint Mary’s Hospital between January 1, 2020, and February 28, 2021. Following the exclusion of 384 patients with an ISS score of ≤ 15 or no reported value, 519 patients with an ISS score of ≥ 15 remained. Of these, 82 patients were discharged from the TICU within 24 hours of admission, 36 patients had a history of pressure ulcers, and 86 patients had ≥ 20% errors in their records and were therefore excluded from the study. Finally, the data of 315 patients were included in this study for analysis.
3. Data collection
3.1. General characteristics
Patient general characteristics, collected from the electronic medical records, included sex, relevant medical specialty, smoking or drinking status, underlying disease (including hypertension, diabetes, and end-stage renal failure), body mass index, critical care triage score, Braden scale score, length of TICU stay, and mortality. The critical care triage score is the mean of the nursing needs of patients admitted to a TICU (it refers to a tool measured by the Critical Care Classification Tool developed by modifying and supplementing the factorial patient classification tool of the United States and the patient classification tool of the Korean Association of Clinical Nurses).
The critical care triage score is a critical care classification tool, each patient’s nursing needs are scored and patients are assigned to one of six groups according to the patient score. It consists of a total of 8 nursing areas and 82 nursing items, and the 8 nursing areas are vital sign measurement, monitoring and measurement, activity, nutrition, intravenous infusion and drug therapy, treatment and procedure (within 30 minutes/ more than 30 minutes), respiration therapy, education, and emotional support. When the nurse inputs values for each item every day for each patient, patients are classified into Groups 1 to 6 according to the total score of the individual items, and the higher the score, the higher the need for nursing care. The score distribution for each patient group is 0 to 13 points for Group 1, 14 to 32 points for Group 2, 33 to 65 points for Group 3, 66 to 98 points for Group 4, 99 to 150 points for Group 5, and ≥ 151 points for Group 6. A Braden scale score 6–9 is classified as the Highest-Risk group, 10–12 is classified as the High-Risk group, 13–14 is classified as the Middle-Risk group, 1518 is classified as the Low-Risk group.
3.2. Characteristics related to trauma
Trauma-related characteristics were collected through the information entered into the Korean Trauma Data Base. Based on the items collected from a previous study, this information was organized into five items: mechanism of injury, trauma type, parts of damage, ISS, and admission route [12].
The ISS is divided into six body regions. AIS scores are assigned to each category, and the top 3 scores with the highest severity score are selected. It is obtained by summing the squares.
In the end, from 1 point for “least severe” up to 75 for “impossible to survive” (unsurvivable), the higher the score, the higher the death rate rises. (It should be noted that if the AIS score is only one area of the body, a score of 6 points results in an ISS of 75 points because it is an unsurvivable injury). When the score is above 15 points, it is accepted as a major or severe trauma. ISS 16–24 points are classified as serious, 25–49 points as severe, 50–74 points as critical, and 75 points as unsurvivable.
3.3. Characteristics related to treatment
Treatment-related characteristics were collected from electronic medical records. Data were based on research tools used in studies by Labeau et al [22] and Kim et al [23], and consisted of 27 items: Glasgow Coma Scale scores at TICU admission, systolic blood pressure, shock status, body temperature, oxygen saturation, surgery, dialysis, ventilator, brace, fixture device, splints, whether or not endotracheal intubation/central venous catheter/peripheral insertion central catheter (PICC)/chest tube/arterial line were used, with or without restraints, sedatives used, inotropic drug used, use of oxygenators (four types other than ventilators), drainage tube, nasogastric tube feeding, duration of ventilator use, and whether a pressure ulcer occurred.
3.4. Pressure ulcer-related characteristics
In patients with pressure ulcers, the following information was obtained from the electronic medical records, and consisted of 8 items: the number of pressure ulcers, days between hospitalization and the development of pressure ulcer, cause, site, stage, size of pressure ulcers, treatment method, and use of air mattress. Pressure ulcers were evaluated according to the pressure ulcer classification system developed by the National Pressure Ulcer Advisory Panel.
Stage 1: Nonblanchable erythema of intact skin. It does not become pale even when pressed.
Stage 2: Partial thickness skin loss involving epidermis and/or dermis. Includes observed abrasions, and blisters.
Stage 3: Full-thickness skin loss involving damage or necrosis of subcutaneous tissue. The epidermis and the dermis are both damaged, and the skin loss was under subcutaneous, but it was not invaded below the fascia.
Stage 4: Wide range of necrosis or damage of a wide range of tissues. Includes muscles, bones or support structures.
Unstageable: The ulcer and the base are completely covered with a nurture or the skin. The depth of the wound and the stage cannot be distinguished until the slough and eschar are removed.
Deep tissue injury: blisters with only color changes to purple or brown without skin damage.
When a patient is hospitalized, the nurse performs a pressure ulcer evaluation within 24 hours. Patients in hospital are regularly re-evaluated once a week, and re-evaluation is conducted when moving between the TICU and the ward, on the day of the occurrence of the pressure ulcer, and when the patient’s consciousness or condition changes. In the TICU, a skin assessment is performed every two hours, periodic position changes are performed, and education pressure ulcer prevention is provided for conscious patients.
4. Ethical considerations
This study was approved by the Institutional Review Board and data collection commenced following approval. All researchers in this study completed research ethics training and complied with their obligations and rules as well as the content of the Institutional Review Board-approved research protocol. Only the researchers could access the collected data, and patient information was anonymously encoded, entered electronically, encrypted, and statistically processed.
5. Data analysis methods
Data analysis was conducted using the SPSS Ver. 14.0 as follows: (1) Patient general characteristics, data on trauma and treatment, and the characteristics of pressure ulcers in the pressure ulcer group were expressed as real numbers, percentage, mean and standard deviation; (2) The differences in general, trauma-related, and treatment-related characteristics between patients with and without pressure ulcers were analyzed by the X2-test, t test, and Fisher’s exact test; and (3) Factors influencing the occurrence of pressure ulcers in patients were analyzed by logistic regression. The goodness of fit of the regression model was assessed using the Hosmer and Lemeshow test.
Results
1. General characteristics of the patients
The general, trauma-related, and treatment-related characteristics of the patients are shown in Table 1. Of the patients there were 245 men (77.8%), and the mean age of all patients was 54.2 ± 17.71 years. The relevant medical specialty was classified as trauma surgery (n = 205, 65.1%), neurosurgery (n = 101, 32.1%), and cardiothoracic surgery (n = 9, 2.8%). Underlying diseases included hypertension (n = 86, 27.3%), diabetes (n = 57, 18.1%), and end-stage renal disease (n = 1, 0.3%). The mean body mass index was 24.40 ± 4.12 of which 137 (43.5%) patients were overweight. The mean critical care triage score was 102.93 ± 20.11, with 183 patients (58.1%) in Group 5 (93–141) and 122 patients (38.7%) in Group 4 (62–92). The mean Braden scale score (a pressure ulcer risk assessment tool) was 10.59 ± 1.85, there were 216 patients (68.6%) in the High-Risk group and 73 patients (23.2%) in the Highest-Risk group. Regarding the trauma-related characteristics, the most frequently occurring mechanism of injury was blunt trauma (n = 303, 96.2%), and the most frequent trauma etiology was traffic accident (n = 155, 49.2%), followed by fall (n = 96, 30.5%), and slip (n = 31, 9.8%). Injuries were divided into six categories as follows: head and neck injuries (included cervical spine; n= 241, 76.5%), thoracic and thoracic spine injuries (n = 189, 60.0%), pelvis and extremities injuries (included lumbar spine; n = 186, 59.0%), skin injuries (n = 183, 58.1%), abdomen and pelvic organ injuries (n = 134, 42.5%), and face injuries (n = 92, 29.2%). The mean ISS score was 25.23 ± 7.97, and the most common route of admission was via 119 ambulance transfer (n = 229, 72.7%). The state of consciousness on ICU admission was categorized as confusion in 87 (27.6%) patients, clarity in 77 patients (24.4%), and coma in 76 patients (24.1%). The mean systolic blood pressure on ICU admission was 122.35 ± 29.60mmHg. Forty-two patients (13.3%) had shock, and patient mean body temperature was 36.23 ± 0.43°C. Following admission, 258 patients (81.9%) underwent surgery; 19 (6.0%) had dialysis; 168 (53.3%) were mechanically ventilated; 249 (79.0%) had a brace; 31 (9.8%) had a fixture device; 138 (43.8%) had a splint; 173 (54.9%) underwent endotracheal intubation; 208 (66.0%) underwent central venous catheterization; 53 (16.8%) underwent PICC insertion; 63 (20.0%) underwent chest tube drainage insertion; 157 (49.8%) underwent A-line insertion; physical restraints were required for 209 patients (66.3%); sedatives were administered to 130 patients (41.3%); 88 patients (27.9%) were treated with inotropes. Forty-two patients (13.3%) developed pressure ulcers. The mean duration of mechanical ventilator use was 4.12 ± 6.28 days. The mean length of ICU stay was 10.17 ± 7.46 days and 41 patients (13.0%) died.
2. Characteristics of pressure ulcer in the pressure ulcer group
The characteristics of pressure ulcers are shown in Table 2. There were 42 (13.3%) patients with pressure ulcers, with a total of 51 sites involved. Of the patients presenting with pressure ulcers, 36 patients (85.8%) developed only one pressure ulcer, while in 6 patients (14.2%) two or more sites were involved. The mean duration from admission to the development of pressure ulcer was 9.74 ± 5.84 days, varying from a minimum of 1 day to a maximum of 23 days. In 14 patients (33.3%) onset was 4–7 days after admission and in 13 patients (31.0%) onset was 8–14 days after admission. Causes of pressure ulcers were immobility in 24 patients (57.1%), unconsciousness in 12 patients (28.6%), and device-related in 8 patients (19.0%). Pressure ulcer sites were the coccyx (n = 21, 50.0%), heels and legs (n = 8, 19.0%), and other areas (n = 6, 14.3%). The pressure ulcer stages were Stage 2 (n = 21, 50.0%) and deep tissue injury (TI = 10, 23.8%). The mean size of pressure ulcers was 2.56 ± 1.26 cm in width and 1.82 ± 0.92 cm in height. Pressure ulcers were treated by conservative management in 42 patients (100.0%) and air mattresses were used for all 42 patients (100.0%) to prevent pressure ulcers.
3. Comparison of characteristics between patients with and without pressure ulcers
3.1. General characteristics
Comparisons of the general characteristics between patients with and without pressure ulcers showed significant differences in age, presence of diabetes among underlying diseases, critical care triage score, length of ICU stay, and mortality (Table 1). The pressure ulcer group contained a greater proportion of patients aged 60–69 years (n = 13, 31.0%) than the non-pressure sore group ( 53, 19.4%; p = 0.009). Diabetes was reported in 13 patients (31.0%) in the pressure ulcer group compared with 44 (16.1%) in the group without pressure ulcers(p = 0.030). There was a significant difference in the critical care triage score between the two groups (111.76 ± 19.55 in the pressure ulcer group vs 101.57 ± 19.88 in the non-pressure ulcer group; p = 0.002). There was a significant difference in the mean length of ICU stay (18.55 ± 9.50 days for the pressure ulcer group vs 8.88 ± 6.17 days for the non-pressure ulcer group; p < 0.001) and in mortality rates (23.8% vs 11.4%; p = 0.031; Table 1).
3.2. Characteristics related to trauma
Among the mechanisms of injury, there was no significant difference in blunt injury between the pressure ulcer group and the non-pressure ulcer group [41 patients (97.6%) vs 262 (96%)]. Regarding trauma type, traffic accidents were reported in 22 patients (52.4%) in the pressure ulcer group and 133 patients (48.7%) in the non-pressure ulcer group and fall in 12 patients (28.6%) in the pressure ulcer group, and 84 patients (30.8%) in the pressure ulcer group, with no significant difference between the groups. The following injuries were reported in the pressure ulcer group and the non-pressure ulcer group: head injuries [33 patients (78.6%) vs 208 patients (76.2%)]; and injuries to the extremities and pelvis [23 patients (54.8%) vs 163 (59.7%)], with no significant differences between the groups. The mean ISS scores were 26.57 ± 8.55 points for with no significant differences in the distribution of each score (Table 1).
3.3. Characteristics related to treatment
Significant differences in the following treatment-related characteristics were observed between the groups: shock (p = 0.001), surgery (p = 0.004), dialysis (p = 0.001), ventilator use (p < 0.001), endotracheal intubation (p < 0.001), PICC insertion (p < 0.001), A-line insertion (p = 0.003), physical restraint applied (p = 0.013), sedative use (p < 0.001), inotrope use (p < .001), nasal cannula (p = 0.042), high-flow O2 therapy (p < 0.001), oxygen tip (p = 0.001), drainage tube insertion (p = 0.009), nasogastric tube feeding (p < 0.001), and duration of mechanical ventilation (p < 0.001; Table 1).
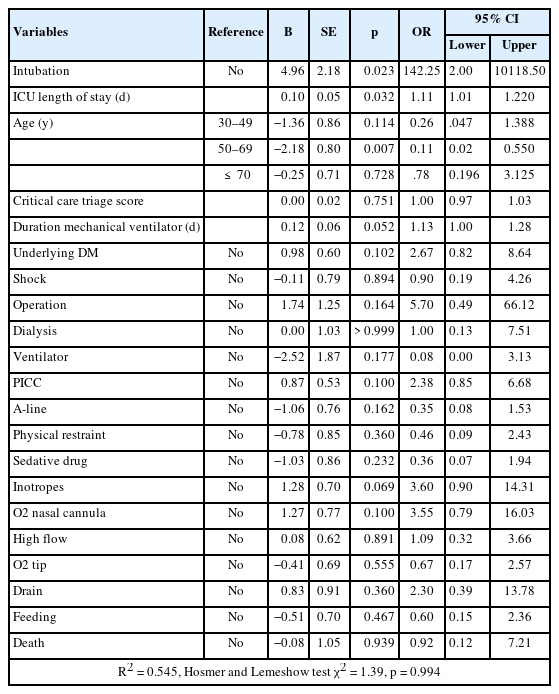
4. Analysis of factors related to the occurrence of pressure ulcers
To determine the risk factors for the development of pressure ulcers, the following 21 characteristics which showed significant differences between the groups in univariate analysis were utilized as independent variables: age, diabetes, critical care triage score, shock, surgery, dialysis, ventilator, endotracheal intubation, PICC, A-line insertion, physical restraint, sedative, inotrope use, O2 therapies, drainage insertion, nasogastric tube feeding, time of mechanical ventilator, length of ICU stay, and mortality. Logistic regression analysis found that the regression model was statistically significant (p = 0.001), with an explanatory power of 54.5% by Nagelkerke’s coefficient of determination. The classification accuracy was 91.7%. The model’s goodness of fit was assessed using the Hosmer and Lemeshow’s method and indicated that data fitted the model well (p = 0.994).
The analysis showed that factors with the greatest effect on the development of pressure ulcers were, in order, endotracheal intubation, length of TICU stay, and age. Endotracheal intubation resulted in a higher occurrence (142.25 times) of cases of pressure ulcers (95% CI: 2.00–10,118.50, p = 0.023). A longer TICU stay was associated with a higher occurrence (1.11 times) of pressure ulcers (95% CI: 1.01–1.22, p = 0.032), while age, between 50 and 69 years, was associated with a lower occurrence (0.11 times) of pressure ulcers compared with the age range ≤ 29 years (95% CI: 0.02–0.55, p = 0.007; Table 3).
Discussion
This study was conducted to determine the characteristics of pressure ulcers in patients with severe trauma who were admitted to a TICU, and to examine the factors affecting the occurrence of pressure ulcers. Of the 315 patients with severe trauma, 42 patients developed pressure ulcers, corresponding to 13.3% of patients. The reported incidence of pressure ulcers in South Korea is from 9% to 17% [12,24], and internationally it has been reported as 28.3% [13]. These results are affected by differences in patients’ general characteristics, trauma type, and treatment characteristics as well as by social and cultural differences.
The mean number of onset days for pressure ulcers in this study was 9.74 days after admission, with most cases occurring between 4 and 7 days. A study by Jung et al [12] reported a mean pressure ulcer onset day of 8.4 days of hospitalization. However, another study in South Korea reported a mean number of onset days for pressure ulcers as 11.14 days after admission, with most cases occurring after 14 days of hospitalization [24]. This difference could be attributable to differences in study design. While the present study was a retrospective study examining medical records, the aforementioned study was a prospective study that identified the onset of pressure ulcers in real time aiming to prevent the occurrence of pressure ulcers.
It has been reported that most pressure ulcers involve the coccyx, consistent with the results of this current study [12,21,24]. Most patients with severe trauma suffer limitation of movement due to multiple fractures. Particularly, in patients with spinal injuries it is important to maintain body alignment, so patients are often in the supine position while wearing a brace. Immobility results in pressure ulcers in the coccyx area where the greatest pressure is applied. For patients on ventilators, the semi-sitting position is recommended for prevention of pneumonia and this position seems to result in pressure ulcers located in the coccyx area [14]. To prevent pressure ulcers, regular repositioning should be performed in accordance with nursing practice guidelines for pressure ulcers, and most frequently affected (taking into account the characteristics of injury in severe trauma patients).
The most frequently occurring stage for pressure ulcers was Stage 2 accounting for 50.0% of all pressure ulcers. A previous study also observed that the most frequently occurring pressure sores were Stage 2 followed by Stage 1 [12]. This current study determined that DTI was the second most frequently occurring type of pressure ulcer injury (23.8%), which was inconsistent with previous studies [12,24]. There may be various reasons for the increased frequency of DTI observed in this current study, despite the application of pressure ulcer preventive foam dressings. However, it seems more important to determine whether pressure ulcer preventive nursing was properly performed. DTIs are likely to worsen pressure ulcers to Stages 3 and 4 later in life if the pressure ulcer is poorly managed [19] so nurses should be trained to actively manage and prevent pressure ulcers, and take measures to prevent deterioration.
In this study, all pressure ulcers were managed with conservative treatment methods (100.0%), and the results were similar to the study by Jung et al [12]. The incidence of pressure sores Stage 1 and 2 was 71.4%, and there were no cases that progressed to Stages 3 or 4, suggesting that they were managed regularly and steadily by a nurse in charge of wounds without surgical treatment such as debris and skin grafting.
The study by Jung et al [12] compared patients with and without pressure sores and found a significant difference in head injury as well as in pelvic and limb injury between the two groups, identifying head injury as an influencing factor for the occurrence of pressure ulcers. Patients with head injuries and multiple fractures are unable to change position on their own due to a decreased level of consciousness. Furthermore, the body’s response to tissue pressure is slowed down, which increases the risk of pressure ulcers. In the case of pelvic and limb injuries, restriction of movement due to wearing splints, fixture devices, or braces increases the likelihood of pressure ulcers [13,15]. However, in this current study, the injury site was not a pressure ulcer influencing factor. Instead, 57.1% and 28.6% of pressure ulcers occurred due to immobility and reduced consciousness, respectively, suggesting that head injury as well as pelvic and limb injury is associated with the occurrence of pressure ulcers.
We postulated that the ISS score would be an influencing factor for pressure ulcers. However, there was no significant difference between the two groups in the ISS score. This finding differed from a previous report [12]. It is important to note that the present study only included severe trauma patients with an ISS score of ≥ 15, which may explain the similarity of trauma-related characteristics among the patients. Furthermore, patients with severe injury may have died before the onset of pressure ulcers, which may explain the results in this current study. Further studies should be conducted to determine whether the ISS score is an influencing factor on pressure ulcers.
Severe trauma patients with acute bleeding often advance into hypovolemic shock (in which systolic blood pressure is measured as < 90mmHg) [14], which reduces systemic and peripheral blood circulation, weakens the resistance to pressure in local tissues of the skin, and lower pressure causes ischemia [14,26], which was thought to increase the incidence of pressure ulcers. However, it does not appear to be an influencing factor for pressure ulcers, as there were many cases of patients with pressure ulcers without shock in this study. In addition, vasopressors, usually used to treat shock, act by constricting peripheral blood vessels to increase blood pressure [14]. It was thought that these actions could further increase the incidence of pressure ulcers as focal ischemia persisted but, considering the results in this study, vasopressors do not appear to directly cause pressure ulcers.
Previous studies showed that the use of surgery, dialysis, ventilators, sedatives, and drainage insertion were risk factors for pressure ulcers [15,19,25,26]. This current study identified endotracheal intubation, length of TICU stay, and age as risk factors for pressure ulcers. In general, hemodialysis should be performed as renal replacement therapy in cases of acute renal injury. Regardless of the underlying disease, patients with severe trauma are hemodynamically unstable when acute kidney damage occurs due to trauma, so vasopressors are often administered, so continuous renal replacement therapy, which is continuously performed for ≥ 24 hours, is applied. In this current study, there was a significant difference between the groups with and without pressure ulcers, but dialysis was performed in only 6.0% of the total number of patients, and there was no difference in trauma-related characteristics between the two groups, so it is believed that dialysis was not a factor affecting pressure ulcers.
The risk of pressure ulcers in severe trauma patients was 142.25 times higher with endotracheal intubation, and 1.11 times higher with long TICU stay, while the risk was 0.11 times lower in patients aged 40 to 59 years compared with the other age groups. Previous studies showed that the use of endotracheal intubation and ventilators increased the risk of developing pressure ulcers [13,14,25]. Generally, endotracheal intubation is accompanied by ventilator use. However, this study identified only endotracheal intubation as a factor affecting the occurrence of pressure ulcers. An increased incidence of pressure ulcers was reported with ventilator use over 20 days [27]. However, in this current study, the mean length of ventilator use in the pressure ulcer group was 11.36 days, which could be due to the reason why ventilator use was not observed as an influencing factor on the occurrence of pressure ulcers. Therefore, if endotracheal intubation is performed, nurses should frequently check and notify the doctor to allow prompt extubation, and prevent the occurrence of pressure ulcers.
A further factor influencing the occurrence of pressure ulcers was the length of ICU stay, which was consistent with the findings reported in a previous international study [20]. TICUs mostly employ invasive and non-invasive medical devices for therapeutic purposes, and the application of these therapeutic devices further reduces the immunity of patients with severe trauma and makes them vulnerable to multidrug-resistant bacterial infections [28]. Infection with multidrug-resistant bacteria requires the use of broad-spectrum antibiotics for treatment, which increases the risk of pressure ulcers due to increased antibiotic resistance and prolonged ICU stay [28]. To reduce TICU stays it is necessary to prevent multidrug-resistant bacterial infections, carefully monitor patients in whom medical devices are used, and actively implement pressure ulcer prevention strategies.
Age was an influencing factor for pressure ulcers in this current study. This was consistent with previous reports identifying the causes of pressure ulcers as decreased tissue circulation, reduced movement, and reduced skin integrity [12,14,27]. The group with pressure ulcers in this study included a greater proportion of elderly patients compared with the group without pressure ulcers. A decrease in subcutaneous fat, skin tissue blood circulation, and sensory function occurs with the aging progress [14,19], promoting the development of pressure ulcers, slow recovery, and leading to the development of more severe pressure ulcers such as Stage 2 or higher. Therefore, preventive nursing activities such as frequently changing patient position and applying preventive foam dressing are important, considering the characteristics of the skin according to age.
In this study, patient characteristics were only examined in relation to TICU admission and TICU stay and not the time when the pressure ulcers occurred, which could be a limitation in identifying factors affecting pressure ulcers. To accurately identify the characteristics of the group with pressure ulcers, it is necessary to examine patient characteristics at the time of pressure ulcer onset. In previous studies, serum albumin, hemoglobin, and nutritional status were determined to be factors influencing the occurrence of pressure ulcers, but these items were not specifically investigated in this current study [14,19,26]. Severe trauma patients are often written up as nothing per oral at admission, so this was not taken into account upon transfer to the TICU. Further research is needed to investigate additional items such as nutritional status when studying bedsores in severe trauma patients.
This study demonstrated that the incidence of pressure ulcers in severe trauma patients admitted to the TICU was 13.3%. We hypothesized there would be an association between the major injury sites and the occurrence of pressure ulcers. However, this was not observed and pressure ulcers appeared to have been caused by a combination of several factors among treatment-related characteristics. TICU nurses should monitor the condition of severe trauma patients continuously for 24 hours, carefully observe the condition of the patient’s skin in whom medical devices are used, and consider the length of hospitalization when performing pressure ulcer preventive care. Furthermore, nurses should apply preventive foam dressings to the pressure ulcer area, and frequently observe the area. Hopefully, the data generated from this study will contribute to future studies on the prevention and management of pressure ulcers in patients with severe trauma.
Conclusion
This retrospective study identified the characteristics of severe trauma patients admitted to the TICU of a general hospital and analyzed the characteristics of the groups with and without pressure ulcers to determine the factors affecting the onset of pressure ulcers. Pressure ulcers were most prevalent in the coccyx region, and the most common stage was Stage 2. Univariate analyses performed to identify risk factors for pressure ulcers showed significant differences in age, diabetes as an underlying condition, critical care triage score, shock, surgery, dialysis, ventilator use, endotracheal intubation, PICC, A-line, physical restraints, sedative and inotrope use, nasal cannula, high-flow oxygen therapy, oxygen tips, drainage insertion, nasogastric tube feeding, length of a mechanical ventilator, length of ICU stay, and mortality. Moreover, logistic regression analysis determined that endotracheal intubation, length of ICU stay, and age were risk factors for pressure ulcer development.
This study analyzed the characteristics of the occurrence of pressure ulcers by assigning severe trauma patients (ISS score of ≥ 15), into groups with and without pressure ulcers. This study provides valuable data allowing TICU nurses to recognize the risk factors for the occurrence of pressure ulcers, and supports the development of pressure ulcer preventive nursing intervention programs.
Based on the results of this study, we make the following suggestions. Firstly, conducting a prospective study to examine whether ISS scores are a pressure ulcer influencing factor. Secondly, repeating this study by expanding the scope of patients, because this study involved severe trauma patients admitted to a TICU in a single general hospital. Thirdly, this study failed to investigate whether a greater number of injured sites increases the incidence of pressure ulcers. Therefore, a follow-up study is required to determine whether the occurrence of pressure ulcers increases with the number of injured sites. Finally, designing future studies on the prevention and management of pressure ulcers in severe trauma patients.
Notes
Author Contributions
Conceptualization: SYL and YMJ. Methodology: SYL and YMJ. Formal investigation: SYL, YMJ, and SYJ. Data analysis: YMJ. Writing original draft: SYL. Writing - review and editing: SYL, YMJ, and SYJ.
Conflicts of Interest
The authors declare that they have no competing interests.
Funding
None.
Ethical Statement
This research did not involve any human or animal experiment.
Data Availability
All relevant data are included in this manuscript.