 |
 |
- Search
| J Acute Care Surg > Volume 13(2); 2023 > Article |
|
Abstract
Fine needle aspiration (FNA) of the thyroid is a well-tolerated minimally invasive procedure. Thyroid abscess, as a complication of FNA in an immune-competent adult, is extremely rare. Diagnosis requires a high index of suspicion, for which treatment is intravenous antibiotics, drainage, and sometimes surgery. Here we present a case of thyroid abscess in an otherwise healthy man who presented with neck pain, rapidly increasing neck swelling, difficulty in swallowing, and hoarseness of the voice that developed two weeks after diagnostic FNA of a thyroid nodule which had been present for ten months. Despite antibiotic treatment, the abscess ruptured into the trachea, requiring surgical intervention. This highlights the importance of maintaining asepsis during FNA of the thyroid. Timely diagnosis of a thyroid abscess is essential to avoid life-threatening airway complications.
Encasement of the thyroid, its rich blood supply, high iodine content, and good lymphatic drainage make it relatively resistant to most infections [1]. Pre-existent thyroid disease, persistence of thyroglossal duct remnant, trauma, or a pyriform fistula predispose immune-competent patients to thyroid abscess. Diagnosis is based on clinical, laboratory, and imaging findings. Staphylococcus aureus is the most common organism cultured from thyroid abscesses [2ŌĆō4]. Rupture of the abscess into the esophagus or trachea is likely to occur in neglected cases. Antibiotic therapy and surgical drainage in conjunction with the removal of any associated anatomical abnormality is usually required. We report a case of thyroid abscess in a 57 year-old immune-competent male following fine needle aspiration (FNA) of the thyroid gland that spontaneously ruptured into the trachea.
A 57-year-old man was referred with a history of dull aching neck pain, rapidly increasing neck swelling over ten days with difficulty in swallowing, hoarseness of voice, and high-grade fever with chills for five days. Two weeks prior, he had undergone diagnostic FNA of a 10-month-old thyroid nodule [ultrasound (US) of the neck had revealed a 4 ├Ś 3 cm, well circumscribed, isoechoic, thyroid imaging reporting and data systems 3 nodule in the right lobe of the thyroid gland and a normal left lobe]. A FNA was performed twice because the first FNA was inconclusive and the cytology report revealed a colloid goiter.
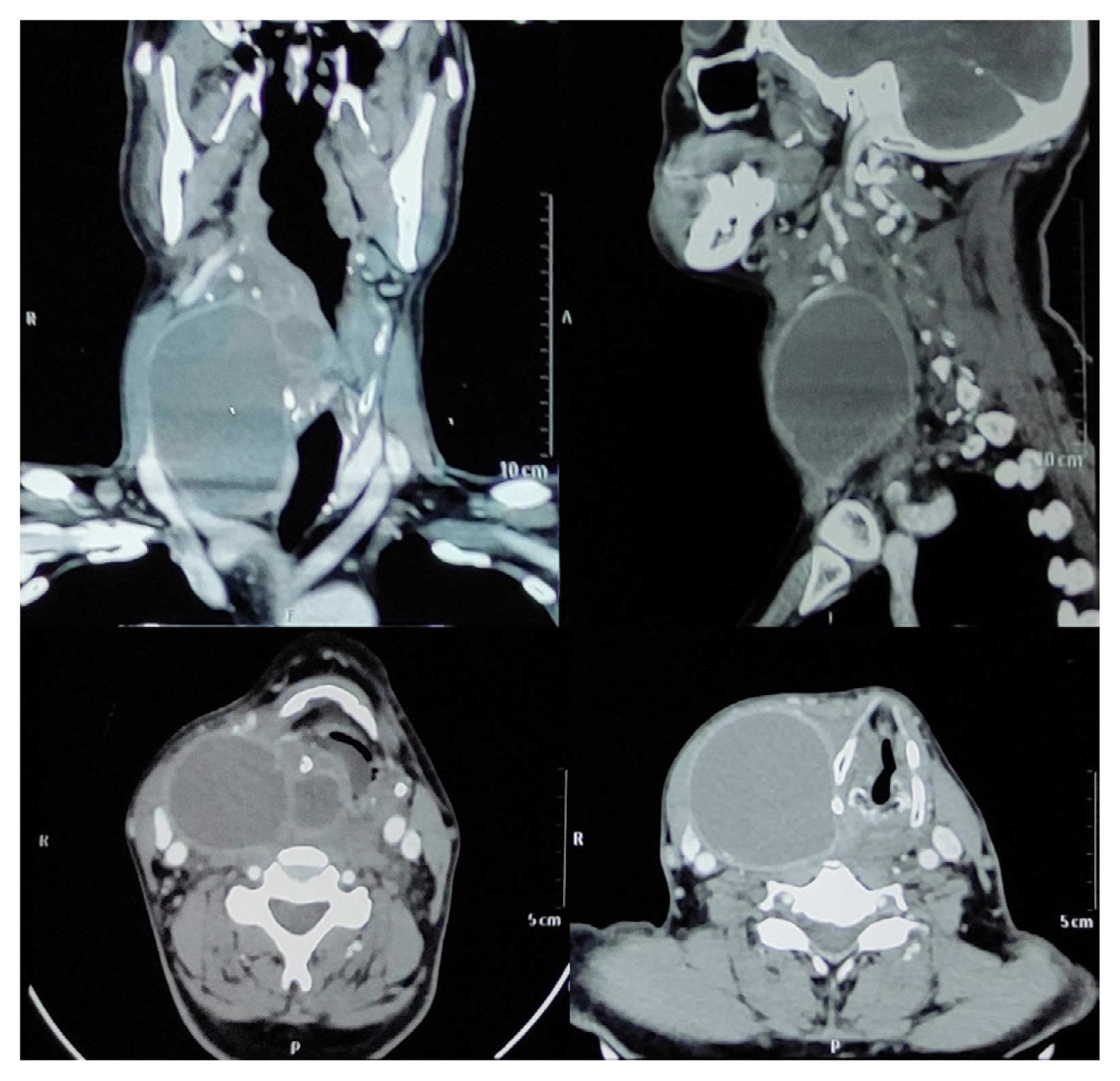
A contrast enhanced computerized tomography (CT) scan of the neck performed at the referring facility where the scan showed a large thick walled, peripherally enhancing, hypo-dense cystic lesion measuring 30 ├Ś 56 ├Ś 77 mm in the right lobe of the thyroid gland extending in the right para-pharyngeal space, compressing the right pyriform sinus with severe narrowing of supra-glottic airway and showing dependent debris within, was suggestive of a large colloid cyst with secondary infection (Figure 1).
The patient subsequently began coughing purulent material and experienced a sudden decrease in the size of the swelling. Thereafter he was referred for further management.
Upon arrival at Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, he was alert, febrile (temperature 39┬░C), with a heart rate of 116 beats per minute, blood pressure of 108/60mmHg, and the room air oxygen saturation was 96%. There was a tense, tender, minimally fluctuant swelling on the right side of the neck which moved with deglutition. The local temperature was raised and the overlying skin was erythematous with no sinus or fistula (Figure 2).
The patient was started on low-flow oxygen, intravenous fluids, amoxycillin 1 g and clavulanic acid 200 mg intravenous injection every 12 hours, and analgesics. US showed a large cystic lesion measuring 7 ├Ś 6 cm with solid components in the right lobe of the thyroid with no flow on color doppler. Bilateral lung fields were clear on the chest radiograph. Laboratory investigations revealed a raised total leucocyte count (16,000/ mm3), and a normal thyroid function range for triiodothyronine (93 ng/dL), thyroxine (6.9 ╬╝g/dL) and thyroid stimulating hormone (1.1 ╬╝g/dL). Arterial blood gas analysis was also within normal range. Flexible bronchoscopy showed redness and inflammation at the second tracheal ring anteriorly. No definite opening or active discharge could be observed. Based on these findings, the patient was diagnosed with an abscess in the right lobe of the thyroid that spontaneously ruptured into the trachea.
The patient was taken to surgery for urgent drainage of the abscess under general anesthesia. Pus and necrotic tissues were removed, and the wound was loosely closed over with a flat drain (Figure 3). During surgery, neither the initial colloid nodule nor any fistulous tract could be defined separately due to intense inflammation. The postoperative period was uneventful. Pus drained at surgery was sent for culture sensitivity study but no growth was observed. The symptoms subsided and the patient was discharged on the 5th postoperative day (after drain removal) with the advice to continue antibiotics for one week. At the two-week follow up, repeat flexible bronchoscopy showed resolution of the previous inflammation with no definite opening, indicating healed tracheal fistula.
Thyroid abscess is an uncommon condition in adults, accounting for less than 0.7% of surgical pathology in the thyroid gland [5]. This is due to the glandŌĆÖs total encapsulation, secluded anatomic position, iodine-rich environment, extensive lymphatic drainage, and abundant bilateral blood supply [1].
Most cases of primary thyroid abscesses have been reported to arise from acute suppurative thyroiditis (AST), an unusual type of head and neck infection [6]. AST has been most often described in children with congenital abnormalities such as pyriform sinus fistula. In adults, the infection is mostly secondary to sepsis [7]. The abscess can also arise in a multi-nodular goiter [8] or a neoplastic thyroid nodule [9]. Local causes can include fish bone injury to the throat [10]. Immune-compromised individuals are particularly predisposed to this condition [11].
FNA of the thyroid is simple, reliable, and well tolerated. Post-FNA local pain and minor hematomas are the most common complications and serious complications are rare [12]. Very rarely there can be direct inoculation of the thyroid from FNA leading to thyroid abscesses [13]. Gram-positive cocci such as staphylococcus and streptococcus are most commonly responsible for thyroid abscesses [2ŌĆō4]. The patients present with painful neck swelling, fever, sore throat and dysphagia. On examination, a firm, tender bulge with overlying warm and erythematous skin is usually detected [14].
Patients have to be hospitalized for monitoring of clinical parameters, biochemical and radiological investigations and intravenous antibiotic therapy. This condition has a variable course and patients may need intubation and controlled pulmonary ventilation or even tracheostomy for airway protection. The peripheral blood picture usually shows leukocytosis [14]. Erythrocyte sedimentation rate and C-reactive protein are raised. Increased thyroglobulin is helpful in identifying the thyroid as a site of inflammation or infection but is not a specific marker for AST [13]. Thyroid function usually remains normal [13]. The patient in this case study had leukocytosis and normal thyroid function.
In most medical centers, CT is the preferred initial imaging modality in the acutely ill patient with suspected AST because it helps to delineate extent and complexity. US is the imaging modality of choice in patients without a compromised airway due to its ability to discriminate the internal anatomy of the gland, and it provides an opportunity for immediate diagnostic and therapeutic aspiration. Thyroid US scans feature in AST include heterogeneous echo-texture of the thyroid gland and development of hypo-to-hyperechoic debris in the thyroid cystic fluid [15]. It is prudent to examine the aspirates and exclude thyroid malignancy that may masquerade as AST. However, the present patient was not advised to repeat FNA due to a previously established diagnosis of colloid goiter.
Antibiotic therapy has to be coupled with drainage of the abscess (needle aspiration, catheter or open drainage) for optimal outcome [11]. Studies recommend penicillinase-resistant penicillin and ╬▓-lactamase inhibitor as initial therapy or clindamycin if there is a history of penicillin allergy. Patients should be shifted to specific antibiotic therapy when microbiological susceptibility data become available. In patients with a known pyriform sinus tract, antibiotic therapy should be continued until elective correction is done [13]. In the current patient, antibiotics which were started empirically were continued in the postoperative period because the culture sensitivity study of the drained pus was negative.
The possibility of pyriform sinus fistula should always be kept in mind in such cases since it might be detected incidentally following thyroid aspiration while misdiagnosing it as traumatic tracheal perforation. The investigations helpful in its diagnosis are laryngoscopy, neck CT or a barium swallow. There are reports describing endoscopic cauterization of the internal opening of the fistula in the same setting of thyroid abscess drainage [16]. However, it may be difficult to identify the fistulae in the acute inflammatory period [17]. Thus, it is best to perform anatomical imaging after abscess resolution, and if present, continue antibiotics, and plan for elective correction of the defect. In the current case no fistulous tract was observed during surgery and during the repeat CT scan of the neck after resolution of the abscess.
Clinical deterioration, abscess persistence despite more than two US-guided aspirations, or abscess progression, should direct therapy to open surgical drainage. The latter entails placement of a small passive drain to prevent continued abscess formation. Urgent transcutaneous or open drainage is recommended for the patient with a compromised airway. In one such reported case, the patient could not be salvaged despite performing a tracheostomy and abscess drainage due to development of aspiration pneumonitis [18]. Thyroidectomy may be required in selected patients with multiple, poorly defined abscesses that progress despite antibiotic therapy and drainage. In previous case reports, management of thyroid abscesses has ranged from sole antibiotic therapy [15,19], to repeated US-guided percutaneous drainage [14,20], CT-guided drainage and catheter insertion [21], open drainage after failed aspiration [6], and open abscess drainage with subtotal thyroidectomy [22]. Keeping in mind the risk of re-rupture of the abscess that could be potentially life threatening, the current patient was taken for urgent open drainage surgery under general anesthesia. Thus, it seems that the management of AST has to be tailored based on the clinical status of the patient, and their response to the treatment.
The exact morbidity and mortality of AST is not known due to its low incidence compounded by under-reporting of typical cases, but patients of AST can have an excellent prognosis if effective antibiotic therapy combined with some drainage procedure can be initiated in a timely manner.
Delay in initiation of treatment, failure of response to treatment, and an immunocompromised state can lead to spreading via fascial planes, retropharyngeal abscess, mediastinitis, septicemia and even rupture of the abscess cavity into the trachea or esophagus [23]. Such patients may need tracheostomy or intubation for airway protection, pulmonary ventilation, extensive debridement, higher up antibiotics, and a prolonged stay in the ICU.
The current patient neither had immune-deficiency nor thyroid malignancy. Since there were no other sources of infection, a breach in asepsis during the repeat FNA seemed to be the likely cause. Coupled with this, delayed presentation led to the abscess rupturing spontaneously into the trachea. Fortunately, the patient improved after urgent open drainage of the abscess. Thus, one should not only adhere strictly to sterile technique while performing FNA but, also have the know-how to promptly diagnose, and adequately manage a rare complication like a thyroid abscess to prevent an even more adverse outcome like spontaneous rupture.
Notes
Author Contributions
Conceptualization, methodology, project administration, supervision, validation, visualization, and writing - review & editing: SM. Investigation, data curation, formal analysis, software and writing - original draft, review & editing: SD, AM, RK, SC, KRM and SKM.
Figure┬Ā1
Contrast enhanced CT scan of the neck suggestive of a large colloid cyst with secondary infection causing severe narrowing of the supra-glottic airway and displacement of the trachea to the opposite side.
References
1. Yeow KM, Liao CT, Hao SP. US-guided needle aspiration and catheter drainage as an alternative to open surgical drainage for uniloculated neck abscesses. J Vasc Interv Radiol 2001;12(5):589ŌĆō94.


2. Berger SA, Zonszein J, Villamena P, Mittman N. Infectious diseases of the thyroid gland. Rev Infect Dis 1983;5(1):108ŌĆō22.


3. Yu EH, Ko WC, Chuang YC, Wu TJ. Suppurative Acinetobacter baumanii thyroiditis with bacteremic pneumonia: case report and review. Clin Infect Dis 1998;27(5):1286ŌĆō90.


4. Jacobs A, Gros DA, Gradon JD. Thyroid abscess due to Acinetobacter calcoaceticus: case report and review of the causes of and current management strategies for thyroid abscesses. South Med J 2003;96(3):300ŌĆō7.


5. Menegaux F, Biro G, Schatz C, Chigot JP. Thyroid abscess. Apropos of 5 cases. Ann Med Interne (Paris) 1991;142(2):99ŌĆō102.

6. Mohamed AA, Al Quarshi TA, Mohamed AA, Saud AM. Thyroid abscess rare complication of thyroid FNA: case report and literature review. Sch J Med Case Rep 2018;6(2):101ŌĆō7.

8. Ameh EA, Sabo SY, Nmadu PT. The risk of infective thyroiditis in nodular goitres. East Afr Med J 1998;75(7):425ŌĆō7.

9. Chen HW, Tseng FY, Su DH, Chang YL, Chang TC. Secondary infection and ischemic necrosis after fine needle aspiration for a painful papillary thyroid carcinoma: a case report. Acta Cytol 2006;50(2):217ŌĆō20.

10. Tien KJ, Chen TC, Hsieh MC, Hsu SC, Hsiao JY, Shin SJ, et al. Acute suppurative thyroiditis with deep neck infection: a case report. Thyroid 2007;17(5):467ŌĆō9.


11. Halenka M, Skodova I, Horak D, Kucerova L, Karasek D, Frysak Z. Thyroid abscess as a complication of fine-needle aspiration biopsy. Endocrinologist 2008;18(6):263ŌĆō5.

12. Polyzos SA, Anastasilakis AD. Clinical complications following thyroid fine needle biopsy: a systematic review. Clin Endocrinol (Oxf) 2009;71(2):157ŌĆō65.


13. Paes JE, Burman KD, Cohen J, Franklyn J, McHenry CR, Shoham S, et al. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid 2010;20(3):247ŌĆō55.


14. Ilyin A, Zhelonkina N, Severskaya N, Romanko S. Nonsurgical management of thyroid abscess with sonographically guided fine needle aspiration. J Clin Ultrasound 2007;35(6):333ŌĆō7.


15. Htet ZW, Tai ES, Yang SP. Acute bacterial suppurative thyroiditis following fine needle aspiration: a case report and review of the literature. Case Rep Endocrinol 2020;2020:7104806.




16. Miyauchi A, Inoue H, Tomoda C, Amino N. Evaluation of chemocauterization treatment for obliteration of pyriform sinus fistula as a route of infection causing acute suppurative thyroiditis. Thyroid 2009;19(7):789ŌĆō93.


17. Miyauchi A, Tomoda C, Uruno T, Takamura Y, Ito Y, Miya A, et al. Computed tomography scan under a trumpet maneuver to demonstrate piriform sinus fistulae in patients with acute suppurative thyroiditis. Thyroid 2005;15(12):1409ŌĆō13.


18. Lee DH, Yoon TM, Lee JK, Lim SC. Vocal cord paralysis and tracheal rupture secondary to thyroid abscess. Surg Pract 2016;20(1):49ŌĆō51.


19. Park JK, Jeon EJ. Infection of Thyroid Cyst Occurring 1 Month after Fine-Needle Aspiration in an Immunocompetent Patient. Int J Thyroidol 2018;11(2):182ŌĆō8.


20. Falhammar H, Wallin G, Calissendorff J. Acute suppurative thyroiditis with thyroid abscess in adults: clinical presentation, treatment and outcomes. BMC Endocr Disord 2019;19:130.




21. Nasa P, Mathew KG, Sanker R, Chaudhary S, Singhal V. Acute Suppurative Thyroiditis with Thyroid Abscess by Klebsiella pneumoniae: An Unusual Presentation. Indian J Crit Care Med 2018;22(8):613ŌĆō15.












