Mortality Trends in Chest-Abdominal Trauma Patients Before and After the Establishment of Trauma Centers in South Korea
Article information
Abstract
Purpose
We sought to assess mortality trends in chest-abdominal trauma patients, before and after the implementation of the Project Supporting Establishment of Trauma Centers (PSETC) in the Republic of Korea.
Methods
Data from the National Health Insurance Service claims database between 2009 to 2017 were analyzed. Patients with chest-abdominal trauma were defined as those with relevant main diagnosis codes and claims for emergency medical management fees. Mortality and cumulative data were analyzed for each year to compare mortality before and after the establishment of regional trauma centers across Korea (2014).
Results
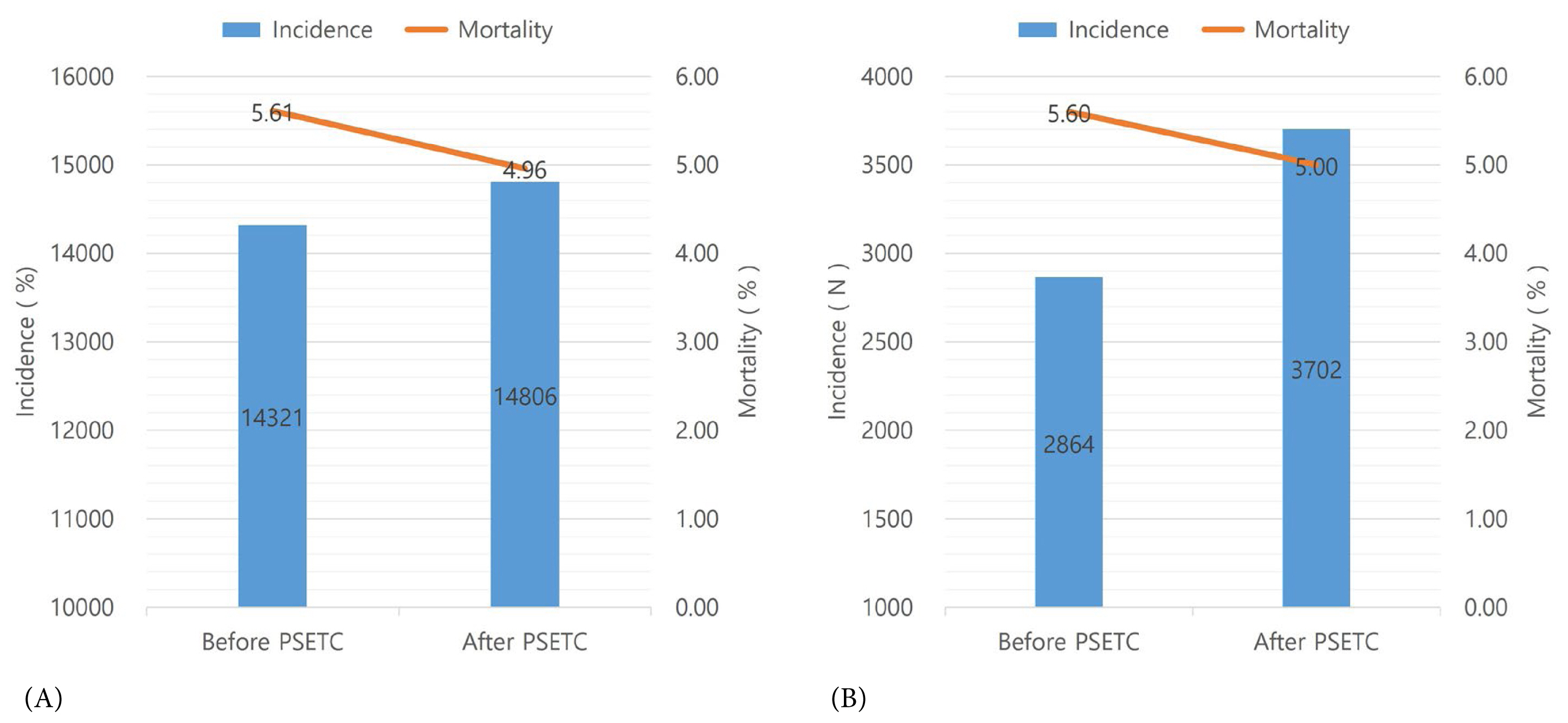
In total, 29,127 patients were included in the analysis. While the annual incidence of trauma-related chest-abdominal injuries increased, mortalities decreased. In particular, the trauma incidence rate among patients over 50 years increased during the study period. Mortalities at trauma centers did not change year by year after the PSETC. Before and after 2014, when trauma centers operated under the PSETC, mortalities decreased [trauma cases before the PSETC; n = 14,321 (mortality 5.61), after the PSETC; n = 14,806 (mortality 4.96)].
Conclusion
The number of patients treated for chest-abdominal injuries increased from 2009 to 2017 in Korea, whereas mortalities decreased over the same period.
Introduction
In South Korea, there are about 120,000 severely injured patients a year, and about 5,000 of them die [1]. The trauma preventable death rate (TPDR) in Korea in 2012 was higher than other nations in the Organization for Economic Co-operation and Development (35.2%) [2]. To address this, the Korean government developed an initiative to support the establishment of regional trauma centers across Korea. The Project Supporting Establishment of Trauma Centers (PSETC) was founded because it had been demonstrated that establishment of trauma center (Level 1) decreased the overall mortality and preventable death rate in the United States [3–5]. Since the installation of these regional trauma centers, the preventable death rate in Korea has been reported to decrease (from 35.2% in 2009–2012 to 30.5% in 2015) [2,6]. The TPDR is calculated based on the sample groups of trauma-related deaths that could have been prevented with appropriated care. The TPDR is a good method to estimate the quality of medical treatment in trauma care. However, it poses several limitations to the study of specific characteristics of overall mortality across Korea [7]. As for the sample group, if the sample size is too small, it becomes inaccurate and unreliable to represent the whole nations’ mortality. According to sample size, the TPDR could be different with overall mortality [2,6]. In addition, reaching consensus views on the TPDR can be difficult, as it is based on the opinions of a panel of experts [8–10]. Comparing surveys on preventable death rate, studies on the overall incidence, mortality, and regional distributions of severe trauma patients across Korea are rare [11].
In South Korea, the national database for trauma patients is not a sufficient source to directly observe the entire population. The National Health Insurance Service Claim database is the only database to deal with information from an entire population of a nation. The goal of the National Health Insurance service claims (NHISC) database is related to insurance for medical treatment. However, the number of patients and mortality rate for trauma patients are reliable because it covers everyone who utilizes the emergency room and pays the emergency medical fee in Korea.
In this retrospective study we sought to document the overall number of trauma patients across Korea and the changes in mortalities before the establishment of trauma centers and after, by using the NHISC database.
Materials and Methods
1. Data sources
This was a nationwide longitudinal cohort study using data from the NHISC database which comprises data on the medical utilization of all Koreans (about fifty million individuals, since 2002). Data include information on the type of medical institutions, date of visit, duration from admission, International Classification of Diseases-10 (ICD-10) codes of treated diseases, type of treatment, results of treatment, and including procedures and medications. Socio-demographic information such as gender, age, and residential province, were included in the NHISC database as well. However, injury severity score, International Classification Injury Severity Score (ICISS), and other severity information were not included. As approximately 98% of the population is included in the national health insurance system in South Korea, claims data are representative of the entire population treated for a specific illness. In this analysis, we used the medical utilization data of patients with chest-abdominal injuries from January 2009 to December 2017, which spans a period before and after the implementation of the PSETC in 2014.
2. Identification of patients with thoracic or abdominal injuries
A patient with thoracic or abdominal injuries was defined as a person diagnosed mainly with the following codes: S25–S29, S31–S32, S35–S39, or S75 based on the ICD-10. Diagnostic codes representing superficial injury (S00–S90, T00, T11, T13–T14), foreign body (T15–T19), burn, intoxication and complication were excluded from this study. Multiple other injuries including brain injury could be overlapped as a sub-diagnosis code, however, these injuries were regarded as minor problems which has a smaller impact on mortality.
The most severe chest-abdominal trauma patients are admitted to the emergency room or trauma-bay after a trauma accident. Therefore, patients with chest-abdominal trauma in this study were defined as those with an appropriate main diagnosis code who were charged for emergency medical management fees upon visitation to the emergency center (or trauma center). The patients who paid emergency medical management fees more than twice or did not pay were excluded from this study.
3. Analysis of outcomes
Analyses were performed using SAS Version 9.4 (SAS Inc., Cary, NC, USA). The Chi-square test and t test were used to determine the type of emergency medical center visited and the characteristics of patients with chest-abdominal trauma. From 2009 to 2017, crude mortalities in each year were calculated according to the type of emergency medical center. The emergency medical institutions were categorized into regional trauma centers, regional emergency medical centers, local emergency medical centers, and local emergency medical facilities. In terms of medical resources, regional emergency medical centers are equipped with more specialized facilities and human resources than local emergency medical centers. In terms of treatment capacity, regional emergency medical centers can provide more advanced emergency medical services to treat more severe emergency patients than can local emergency medical centers. The regional trauma center is an emergency medical institution with medical staff and treatment systems optimized for treating severe trauma patients and most trauma centers are located near to a regional emergency medical center, although this can differ from region to region (Figure 1A).
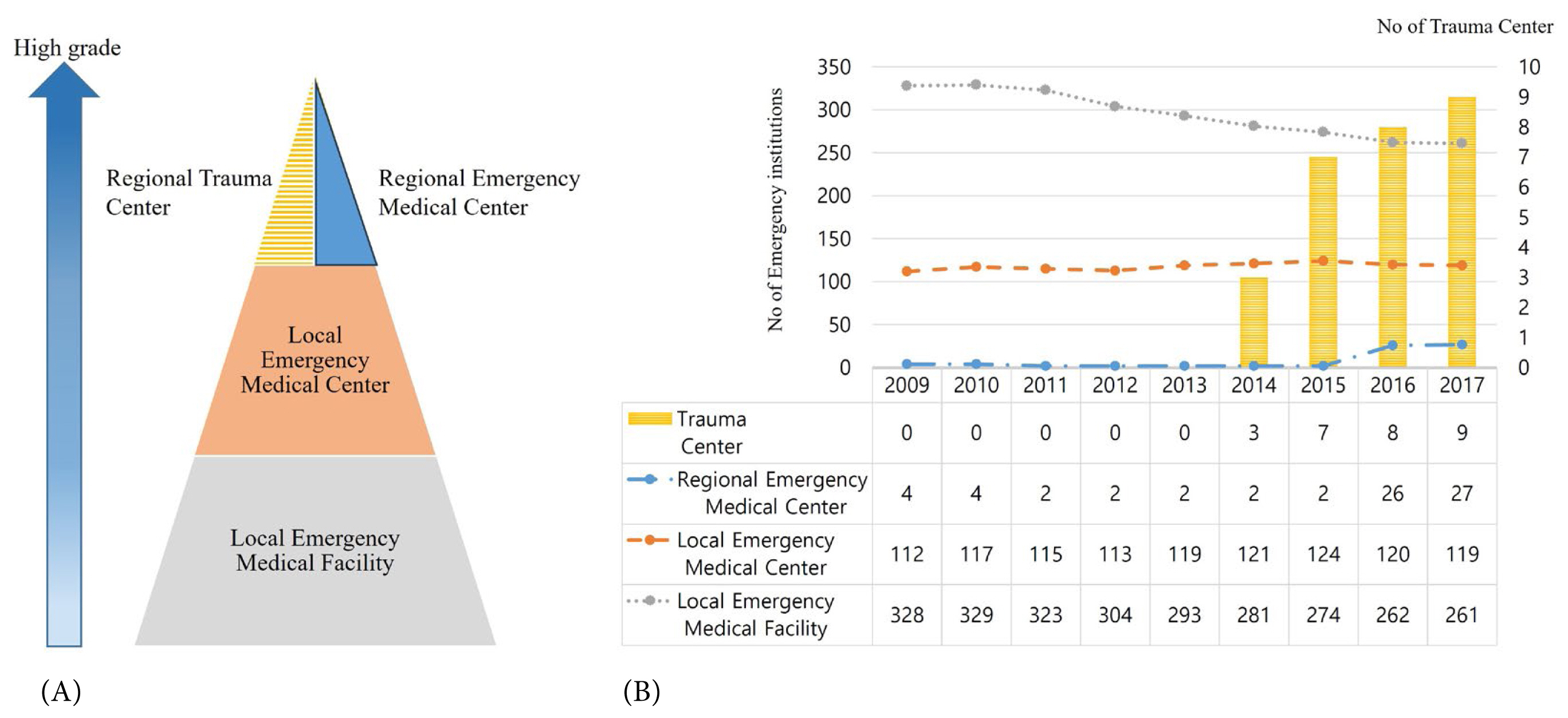
(A) Classification of emergency medical institutions and regional trauma centers according to the level of medical treatment in Korea. (B) The number of emergency medical institutions and regional trauma centers categorized by year.
Since the first designated trauma center became fully operational since 2014, the pre-trauma-center period was defined as 2009 to 2013, and the post-trauma-center period was defined as 2014 to 2017 (Figure 1B) [12]. Cumulative data for each year were investigated to determine changes that occurred as a result of implementation of the PSETC (the initial operational dates for the trauma centers varied regionally).
Results
1. Annual trauma incidence and mortality
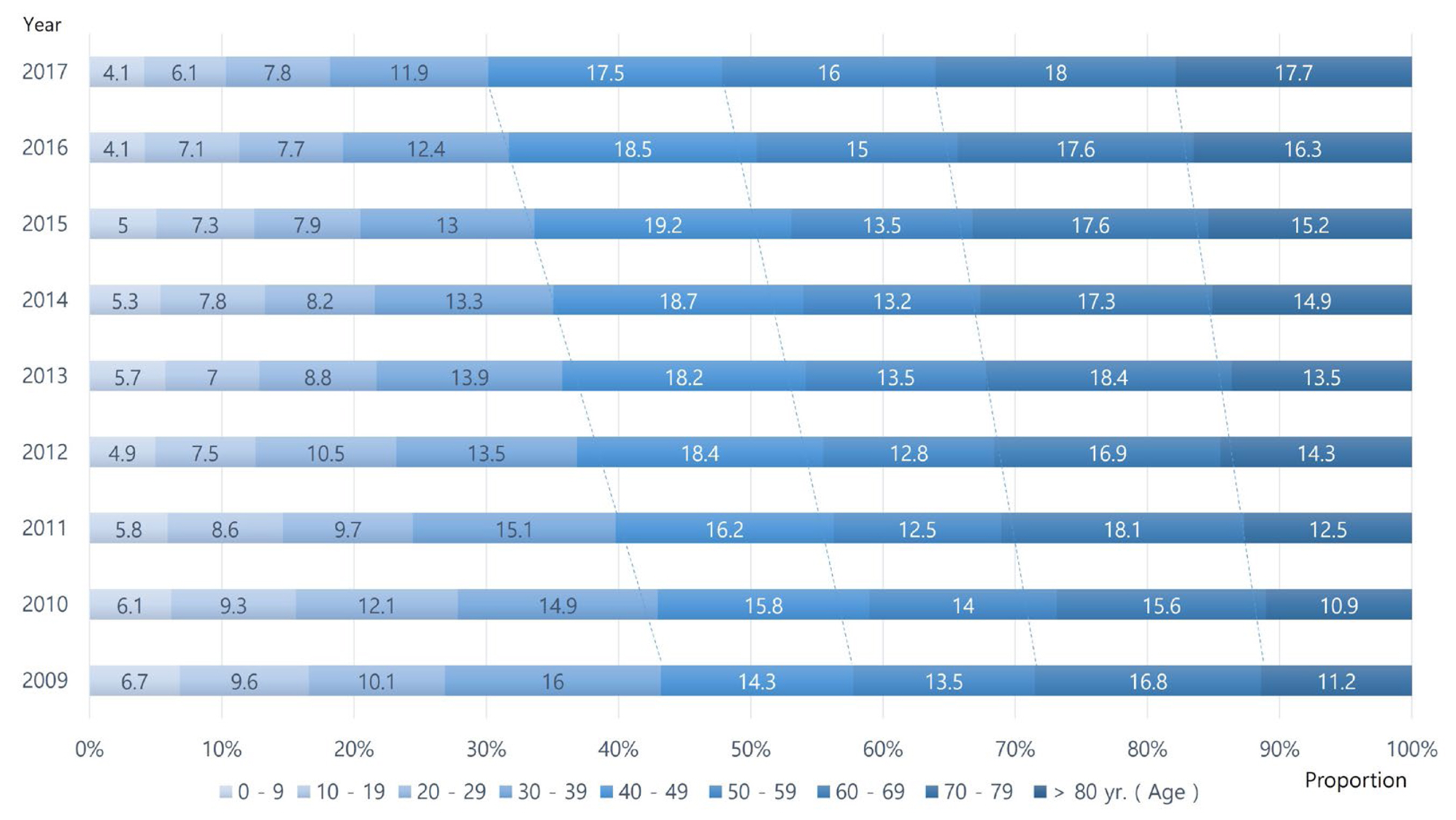
A total of 170,749 patients with thoracic or abdominal injury codes were registered with the National Health Insurance Service during the period from 2009 to 2017. Among them, there were 140,937 patients who were excluded because they did not pay emergency medical care fees, or paid fees more than twice. Therefore, in total 29,127 patients were included in the study: 27,589 survived and 1,538 died in the emergency department (Figure 2). Overall, during the period 2009–2017, the annual incidence of trauma increased, whereas mortalities of trauma decreased (Figure 3). When the occurrence of thoracoabdominal injured patients was investigated by age group, the proportion of patients aged 50 or older increased as the years passed (Figure 4).
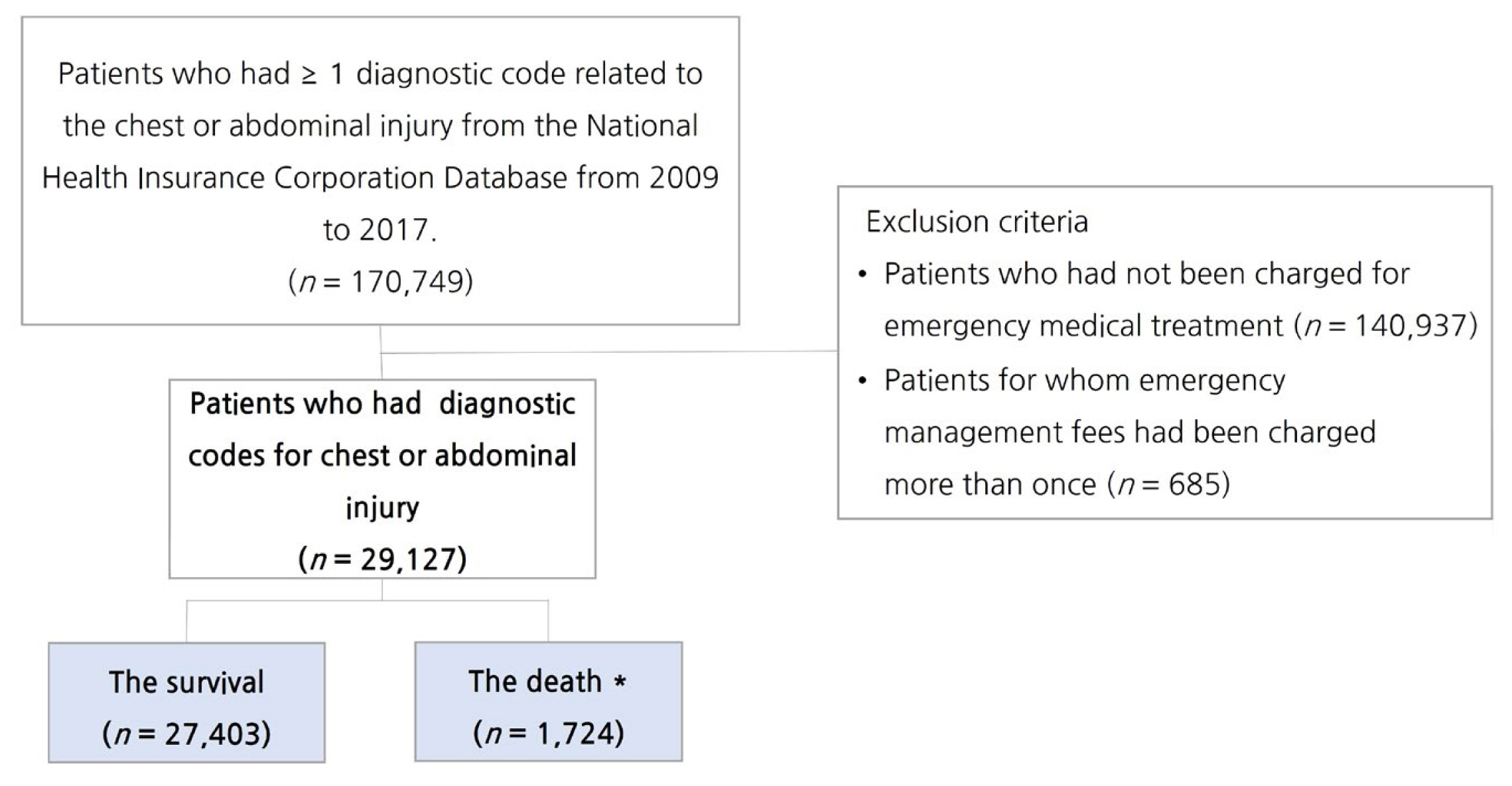
Flowchart of patient inclusion in this retrospective study. In total, 29,127 patients were included after excluding patients who had contraindications from all 170,749 patients with a chest or abdominal injury code.

Overall incidence and mortality of trauma patients with chest-abdominal injuries. While incidence increased, mortality decreased.
2. Trauma patients and mortality among emergency medical institutions
During the target study period, 1,423 (4.89%) patients visited trauma centers, while 5,559 (19.1%) visited the regional emergency centers. Most trauma patients (14,509 patients, 49.8%) visited local emergency centers, and 7,636 (26.22%) visited local emergency facilities (Table 1).
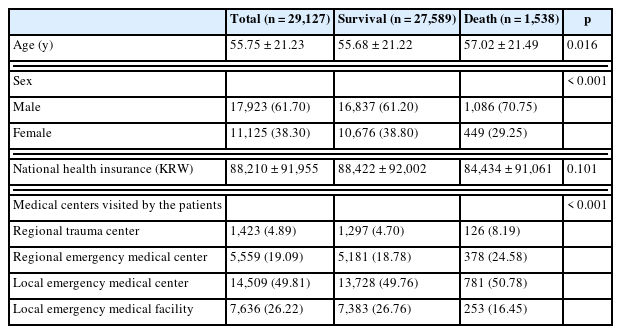
Demographics for thoracoabdominal trauma patients and death tolls according to emergency medical institution
The number of chest-abdominal trauma patients rose steadily year on year in all medical institutions. Since trauma centers began operating in 2014, thoracoabdominal trauma patients were categorized as being treated at a regional trauma center, regional emergency center, local emergency center, or local emergency facility from then on (Table 2).
3. Trauma patients and mortality before and after the PSETC
The PSETC began in 2013, and the full-fledged opening of regional trauma centers began in 2014. Therefore, to determine the impact of these trauma centers on trauma-related mortality, the number of patients treated and deaths before and after 2014 were compared. The mortality in emergency room were higher before the PSETC [n = 14,321 (mortality rate 5.61)] than after [n = 14,806 (mortality rate 4.96); Figure 5A]. The annual incidence after the PSETC was higher than that before the PSETC. The annual mortality after the PSETC was lower than that before the PSETC (Figure 5B).
Discussion
In South Korea, about 120,000 people are severely injured annually, of which about 5,000 people die [1]. Despite ranking as the top cause of death in young Koreans, posing large social and economic losses, there are little data on the incidence, mortality, and regional distributions of severe trauma patients [11]. This study outlines changes during 2009–2017 in trauma-related mortality and incidence before and after implementation of the PSETC, a nationwide project supporting the establishment of regional trauma centers across South Korea using NHISC data which reflects 98% of the population of Korea.
The TPDR, which is often a cited measure of treatment quality in trauma-related events, poses limitations to the evaluation of overall trauma mortalities. To reliably represent the mortality rate of the entire population sample sizes must be extensive if using the TPDR because assumptions are made when using parametric tests. A previous study using the TPDR to determine treatment quality in trauma-related events in Korea (2009–2010) had such limitations as a lack of sample groups representative of traumatic patients across the country, as Difficulties in standardizing medical views and evaluation criteria among researchers, and as evaluations of causes of death based solely on imaging and medical records, not autopsy reports [2]. Most importantly, the TPDR is generally defined as the rate of death among individuals who would have survived if they had been transported to an appropriate care facility within an appropriate time and received appropriate treatment, thus making it largely a measure of treatment quality [13]. Accordingly, TPDRs can be different from actual death rates, and a decrease in the TPDR does not necessarily reflect a decrease in overall mortality. In this current study the simple pattern of change in the majority of the population of Korea who sustained severe trauma in the torso area during 2009–2017 [trauma-related thoracic or abdominal injuries (29,127) and mortalities (1,537)] was assessed.
In this study, despite continual increases in thoracic or abdominal injuries, the mortalities decreased from 2009 to 2017. Most studies which have attempted to document the causes of increased events of chest or abdominal trauma in Korea are based on local data or cover a study period limited to a few years. One retrospective study reported that the gradual increase in the number of trauma cases could be due to accelerated individualization, increased use of transportation, and increased participation in leisure activities [14]. However, statistics from the Ministry of Transportation indicate that traffic accidents, which account for the majority of trauma mechanisms, have continued to decline over the past decade, and resultant mortalities have also declined. As such, this would not explain the observed increase in the number of patients suffering from chest-abdominal trauma [15]. However, the fact from Statistics Korea that patients transported by 119 rescue teams increased every year affected incidence by increasing the diagnosis rate at the emergency room stage [16]. Meanwhile, increase in trauma injuries has been similarly reported overseas. A study in the UK 1997–1998 determined that the increase in ambulance transport is related to an aging population, increased chronic diseases, and improvement of ambulance service [17]. Researchers in Spain reported that although traffic accidents decreased, the total number of trauma events increased from 2000 to 2010 [18]. They also noted that trauma events in older adults had a substantial impact on overall trauma rates. In the United States, similar to our study, the incidence of trauma increased between 2000–2011, while mortalities decreased [19]. Although research has yet to determine exactly why trauma cases are increasing, several studies have drawn links between increases in trauma and aging populations and declining birthrates [16,18,20,21]. Likewise, when we looked at changes in the incidence of trauma patients according to age group in this study, increases in trauma incidence rates followed a gradual increase in the proportion of individuals aged 50 years and older (Figure 4).
The reduction in mortality over time may have multiple reasons. However, it is also difficult to exclude the link with quality improvement of trauma care. Two national reports in 2012 [2] and 2019 [6] have documented decreases in the preventable death rate for trauma and a drop from 30.5% to 21.9% was reported [6], which is likely due to improvements in medical treatment and medical facilities dedicated to trauma in South Korea. Actually, several reports in the Republic of Korea reported that the quality of medical treatment had improved after the operation of trauma centers [22–24]. In addition, a reduction in preventable death rates combined overall mortalities decreased with the operation of trauma centers [3–5]. Mortalities for severe trauma injuries in the United States decreased from 14.1% to 8.9% after upgrading 1 trauma center from Level 2 to Level 1 [5]. In Austria, overall mortalities decreased by 8% after the opening of a trauma center [25]. Accordingly, we would find it difficult to exclude a link between qualitative improvement in trauma-related health care (under support from the Korean government to establish regional trauma centers) and the observed reductions in mortalities. However, it is difficult to conclude an accurate reason for decreased mortality rate in this current study.
Since the PSTEC and the start of the trauma center, the transport of trauma patients for emergency care has been dispersed from emergency institutions to include trauma centers. As the number of trauma centers opening after 2014 increased compared with the period from 2009 to 2013 before the development of trauma centers, the mortality at some emergency institutions (e.g., regional emergency center and local emergency medical facility) showed an overall tendency to decrease, and the mortality at trauma centers showed an increasing trend. We do not know the reason for this change-pattern only in this data information, but it is thought that since the PSETC, the trauma centers may have relieved the burden on other institutions for the severely injured patient such as the thoracoabdominal trauma patients which were included in this study. Regional trauma centers are superlative in the trauma field and transfer of severely injured patients to other hospitals is not permitted by the government of Korea. This suggests that thoracic or abdominal injured patients, who have been transported to various hospitals in previous years, are now being transferred to trauma centers and the severity of the patient in a trauma center may be high. This is the new normal because there have not been special hospitals for severely injured trauma patient before the PSETC in Korea. Although we would not confirm the severity of trauma and transfer status of patients accurately in this study because the claims database did not have enough information. Nevertheless, compared with other emergency medical institutions, trauma centers specializing in treating trauma patients have been reported to show lower preventable death rates (trauma center 21.9%; emergency medical institution, 33.9%; OR 2.13), and Z and W scores (Z score; it indicates the statistical significance of the difference between the number of actual versus expected survivors, W score; It describes the number of unexpected survival outcome per 100 patients) have reportedly risen after the opening of regional trauma centers [3,22,24]. Caring for the majority of severe trauma patients in the trauma center facilitates an increase in the survival rate of severe trauma patients which was the purpose of establishing the trauma center. Therefore, this should be emphasized more as a role of the trauma center in the future.
Despite the establishment of trauma centers where better care is available, the lack of improvement in mortalities at trauma centers may stem from inefficient trauma systems. Indeed, studies have indicated that Korea’s trauma systems have not improved transfer times to the final hospital, the appropriate selection of transfer hospital, and there has been no provision for a dedicated department to mediate between hospitals, or between hospitals and the scene of the accident, all of which may act as reasons for the steady mortalities at trauma centers [6,24]. Accordingly, cultivating a cooperative, community-based approach to managing emergency care, such as that emphasized in the “Model Trauma System Planning and Evaluation” (a document published by the Ministry of Health and Welfare, in the United States), could prove beneficial to reducing trauma-related mortalities [26]. As an important aspect to this, creating and operating a separate administrative body to act as an intermediary for multi-agency ministries (Ministry of Health, Welfare, Police, and Metropolitan Government) related to the trauma sector has been proposed in the United States [27,28]. The state of Maryland in the United States has employed an independent administrative institution (Maryland Institute of Emergency Medical Service System) since 1993 to coordinate all components of its statewide emergency medical service, including transportation, operation, research, and education, in accordance with Maryland statutes and regulations [27]. In 2016, the National Academy of Sciences in the United States reported that a national trauma system must be established to achieve zero preventable deaths after injury [29]. They emphasized that there must be unified system of injury care for improving preventable death rates under leadership at the highest levels of the Department of Defense and the Federal Government.
In South Korea, even though there has been the establishment of trauma centers, a well-organized trauma system should be established. It was attempted as a pilot project supported by the Ministry of Health and Welfare of Korea in 2018. This project emphasized cooperation and developed a protocol that could be shared among trauma-related institutes. The protocol emphasized ongoing management and governance of an interconnected trauma system. Further development of trauma management systems would help reduce overall mortalities in Korea.
This study has several limitations that warrant consideration. One limitation is the retrospective design of the study. Additionally, although the number or range of data in the National Insurance Claims database is vast, the nature of the claims database was not specific for trauma research. The database did not detail information on the severity of the clinical conditions of the patients and the other organs involved as an outcome of the trauma, at the time of admission. Moreover, although the distance and duration from the site of the emergency to the hospital can affect the clinical outcomes of patients with thoracic or abdominal trauma, actual transfer modes (ambulance, helicopter), distances, and times could not be determined due to the nature of the data. In addition, reduced mortality because of development of overall medical care, social community activation, and informatization cannot be clearly excluded in this study.
In the Republic of Korea, the number of the trauma patients who sustained chest-abdominal injuries and were treated in an emergency room increased from 2009 to 2017. Over the same period, however, mortalities for trauma-related events decreased in the same period.
Notes
Author Contributions
Conceptualization: HS and JYJ. Methodology: DRK, HSK, and HS. Formal investigation: HSK. Data analysis: HSK and DRK. Writing original draft: HS. Writing-review and editing: JYJ, OHK, KK, UYC, JK, and KSB.
Conflicts of Interest
Ji Young Jang is an editor of this journal but this had no influence in the decision to publish this article. There were no other potential conflicts of interest relevant to this article.
Funding
This research was supported by research funding for new faculty from Yonsei University Wonju College faculty of Medicine.
Ethical Statement
This study incorporated analysis of secondary data from the National Health Insurance Service. The data did not include identifiable information, such as name, address, or phone number. Only non-identifiable aggregate results that were openly available for public research purposes were released and informed consent could not be obtained.
Research plan and protocols were reviewed and approved by the institutional review board of Yonsei University Wonju College of Medicine (IRB no.: CR319310).
Data Availability
All relevant data are included in this manuscript.