Introduction
Pancreatic injury caused by blunt trauma is rare, and isolated pancreatic injury is rarer [1]. Such injuries result in high morbidity and mortality rates usually due to delayed diagnosis and treatment [2]. Early diagnosis of pancreatic injury is challenging because of its presentation and subtle symptoms due to the retroperitoneal location of this organ. Generally, low-grade pancreatic injury can be nonoperatively managed. However, operative management is recommended for high-grade injuries, involving main pancreatic duct (MPD) [3]. Certain studies have demonstrated increased morbidity and mortality because of delayed surgery in patients with high-grade pancreatic injuries who initially nonoperatively treated [4]. However, due to the development of intervention skills and intensive care, nonoperative management, including endoscopic and radiologic intervention has become a promising treatment option in recent years [5].
We report a case of isolated transection of the pancreatic neck after blunt trauma that was successfully managed with endoscopic stenting.
Case Report
A 16-year-old boy was transferred to the regional trauma center of Pusan National University Hospital after a motor vehicle accident. He complained of mild abdominal pain and focal tenderness in the epigastric area. Initial vital signs were stable; blood pressure 120/80 mmHg, heart rate 106/min, and respiratory rate 16/min. Laboratory findings were significant for white blood count 20.49/Îźl (reference range, 4,000âź 11,000/Îźl), mildly elevated amylase 102 IU/L (reference range, 36âź128 IU/L), and lipase 220 U/L (reference range, 22âź51 U/L) and other values within normal range.
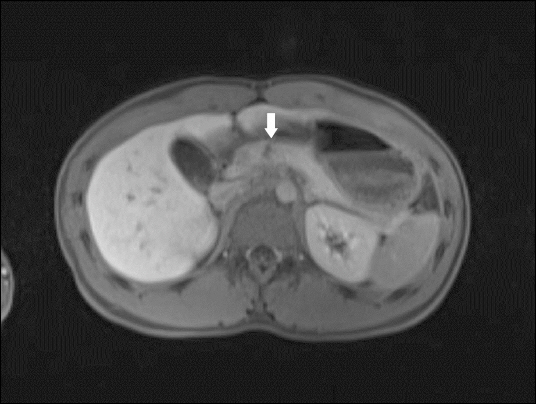
Abdominal contrast enhanced computed tomography (CT) revealed transection at the neck of the pancreas with a small peripancreatic fluid collection (Fig. 1). No evidence of other intra-abdominal organ injury was found. Magnetic resonance cholangiopancreatography (MRCP) of the pancreatic duct was indicative MPD injury (Fig. 2). His vital signs were stable, abdominal pain was less than moderate, and he had no other intra-abdominal organ injury. Therefore we decided on nonoperative management and the patient was admitted to the trauma intensive care unit. Surgical treatment was also planned if the patient did not receive endoscopic retrograde cholangiopancreatography (ERCP) within 24 hours, the procedure was failed or the patientâs condition was aggravated.
Fig. 1
Computed tomography of abdomen suggesting transection at the neck of the pancreas with small amount of peripancreatic fluid collection (arrows).

Fig. 2
Magnetic resonance cholangiopancreatography showing transection at the pancreas neck (arrow).
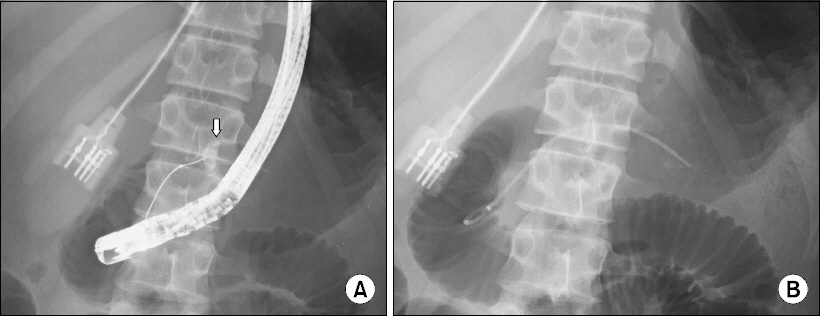
The next day, ERCP, performed within 24 hours after injury for evaluation and nonoperative management of the MPD injury, demonstrated complete disruption of the MPD on the neck (Fig. 3), which is a grade III injury according to the American Association for the Surgery of Trauma. A 5 French stent was placed to cross the injured site. On day 3, follow-up CT scan demonstrated no significant interval change. After intensive care of four days, the patient was transferred to the general ward for conservative care. On day 10, follow-up CT scan showed no interval change, and enteral feeding was started. On day 17, follow-up CT was similar as before, and he was discharged without any significant complication 18 days after the trauma.
Fig. 3
(A) Endoscopic retrograde cholagiopancreatography demonstrating pancreatic duct complete injury with contrast leakage (arrow). (B) A pancreatic stent was placed to cross the injured site.
On day 33, CT scan revealed reduction of the peripancreatic fluid collection. On day 34, a second ERCP demonstrated contrast leakage from the injured site of the pancreatic duct, so the stent was changed. The patient remained stable and did not show any other symptom. Lastly, the third ERCP on day 99 revealed no contrast leakage. The fluid collection also was reduced on follow-up CT scan. After four days, on day 103, we successfully removed the stent. The patient was followed-up in the outpatient clinic without any significant complication.
Discussion
Pancreatic injury is rare, occurring in 3.1% of blunt abdominal traumas, and isolated pancreatic injury is rarer (0.7% of blunt abdominal traumas), but they are associated with morbidity and a mortality rate s of up to 12% and 34% respectively [1,2]. Because of the proximity of adjacent solid and hollow organs and vascular structures, associated injuries are common [6]. Due to the retroperitoneal location, clinical signs and symptoms are initially vague and subtle. In addition, there is no laboratory finding that is specific for pancreatic injury. Therefore, delayed diagnosis is common and leads to high morbidity and mortality rates, especially in patients with MPD injury. Early diagnosis of MPD injury is most crucial after blunt pancreatic trauma.
For blunt pancreatic injury, abdominal CT scan (contrast enhanced) is the first choice of image study. However, during the early period after trauma, the sensitivity and specificity of CT scans for MPD injury are not satisfactory [7]. When CT findings are inconclusive but suspicious according to the injury mechanism, further investigation with other image studies or procedures should be conducted. Next, if the patient is hemodynamically stable, the pancreatic injury is not significant and there is no other intra-abdominal organ injury, MRCP or ERCP can be performed. MRCP allows for noninvasive evaluation of not only the integrity of the pancreatic duct but also pancreatic parenchyma and the surrounding tissues [7]. Despite its own complications, we prefer ERCP because it can be performed with the possible stenting of the MPD. We could find the pancreatic injury on the initial CT scan, but it was necessary to identify the presence of main duct injury. If there is a main duct injury, operative treatment or endoscopic intervention should be performed within 24 hours to achieve good results. Once the patient was young and the symptoms were mild and there was a small amount of fluid collection around the pancreas, we considered non-operative treatment first. However, there are not many hospitals where ERCP is available 24 hours a day, 365 days a year. In our institution, one endoscopic interventionist is in charge of the entire hospital. Therefore, generally, ERCP Can be performed only during daytime on a specific day of the week (monday, wednesday, and thursday), and the procedure was not performed within 24 hours as routine. After identifying the main duct injury with MRCP, we consulted with the interventionist and ERCP and pancreatic stent insertion was able to be performed emergently on the day when the procedure was not possible routinely.
ERCP is considered the golden standard for the diagnosis of the pancreatic duct injury. ERCP reveals the integrity of the pancreatic duct and the injured site and extent; thus decisions for the appropriate method of management are possible. According to the condition of the injury, endoscopic treatments, such as stenting to bridge the injured site and sphincterotomy can be simultaneously performed.
Controversies regarding the operative or nonoperative treatment of grade III or IV pancreatic injury exist. Regardless of the grade III or IV injury, the primary challenge is restrict MPD leakage. In their guideline for management of adult pancreatic injuries, the Eastern Association for the Surgery of Trauma recommends operative management for grade III or IV pancreatic injury. They stated that treatment delays likely contribute to morbidity and mortality due to regularly occurring treatment failure after nonoperative treatment [3]. However, due to the development of intervention skills and intensive care, successful nonoperative management for pancreatic injury have increased.
Bhasin et al. [4] recommend that patients with duct disruption, especially partial, that can be bridged should undergo transpapillary pancreatic duct stenting. However, patients with complete duct disruption should be surgically treated. Recently, several cases of successful treatment of grade III pancreatic injury with endoscopic management have been reported [8]. Further studies are required for confirming whether nonoperative management improves morbidity and mortality.
Lin et al. [9] reported the long-term results of endoscopic stenting for blunt major pancreatic duct injury. In their study, three of six patients had severe MPD stricture as a complication of stenting or the injury itself and the stent was maintained for a long duration (26âź43 months). Our patient was asymptomatic for the seven months of follow-up and needs long-term observation.
Other concerns regarding nonoperative management of pancreatic injury include post-ERCP pancreatitis and the requirement of additional intervention. Presently, the definition of post-ERCP pancreatitis is widely accepted fulfillment of two or more of the above three criteria: a serum amylase and or lipase level at least three times the upper limit of normal range in the presence of abdominal pain and/or radiologic findings of inflammation of the pancreas [10]. In the present case, the pancreatic enzyme level was elevated after ERCP but the patient did not complain of abdominal pain. After few days, the elevated pancreatic enzyme normalized. Multiple ERCPs and endoscopy for stent removal could potentially harm the patient. Our patient underwent three ERCPs and finally endoscopy for stent removal without significant complications. However, the patient avoided laparotomy under general anesthesia and complications of pancreatic resection.
Isolated pancreatic transection is rare and is traditionally managed by laparotomy. However, we successfully treated an MPD injury with ERCP and stenting. In selected patients, endoscopic treatment can be an attractive therapeutic option, avoiding the requirement for laparotomy.








