Preperitoneal Pelvic Packing Prior to Pelvic Angiography in Patients with Hemodynamic Instability due to Severe Pelvic Fracture: Two Cases
Article information
Abstract
The mortality of patients with hemodynamic instability due to severe pelvic fracture is high despite multidisciplinary management. Current management algorithms for these patients emphasize pelvic angioembolization (AE) for hemorrhage control. However, a surgical procedure is often needed because AE is time-consuming and approximately only 15% of patients have arterial bleeding. Most hemorrhages from severe pelvic fracture originate from venous or bone injury. Current research demonstrates the effectiveness of preperitoneal pelvic packing (PPP) in hemorrhage control. However, there are no reports of its use in Korea. Accordingly, we present our early experiences of PPP for control of hemorrhage due to severe pelvic fracture in a trauma center in Korea.
Introduction
The mortality rate of trauma patients with hemodynamic instability due to severe pelvic fracture is reported to be over 40% in spite of increased awareness and early management by a multidisciplinary team [1]. Current management algorithms for unstable pelvic fracture emphasize pelvic angioembolization (AE) for hemorrhage control [2,3]. However, AE is a time-consuming procedure because patients have to be transported to the interventional radiology room and time for preparation of paramedics and staff is needed. In addition, approximately 85% of hemorrhages from severe pelvic fracture are caused by bleeding from venous plexus and bony fracture site, and only 15% are from arterial injury [4]. For these reasons, several studies on preperitoneal (retroperitoneal) pelvic packing (PPP) in unstable pelvic fracture have been reported since the mid-2000s [5-7]. These observational studies or case series showed that PPP was very effective in the control of acute hemorrhage due to severe pelvic fracture. In particular, Burlew et al.[7] reported that early PPP prior to AE was successful in bleeding control of unstable patients with severe pelvic fracture. In this study we describe our early experience of PPP in a single trauma center in Korea.
Case report
Case 1
A 56-year-old male found crushed under an overturned car was sent to the trauma center. Initial vital signs upon check-in at the trauma bay were blood pressure of 79/61 mmHg, pulse rate of 123/minutes, and body temperature of 34°C. His mental status was stupor. There was bleeding from the left ear and swelling of the pelvic area. Focused assessment sonography for trauma was negative. Fractures in both superior and inferior rami and left sacroiliac (SI) joint and a large amount of hematoma in the pelvic area were identified in an abdominopelvic computed tomography (APCT) scan (Fig. 1). Brain computed tomography showed basal skull fracture, pneumocephalus, and temporal bone fracture. Injury severity score was 50. Initial arterial blood gas analysis (ABGA) indicated severe metabolic acidosis (pH 7.023, base excess -19.2 mmol/L, and lactate 11.14 mmol/L) and hemoglobin was 9.1 g/dl. Although 4 units of packed red blood cells (RBC) were transfused after intubation and central venous catheter insertion, he was sent to the hybrid operation room (OR) because of persistent shock 40 minutes after admission.
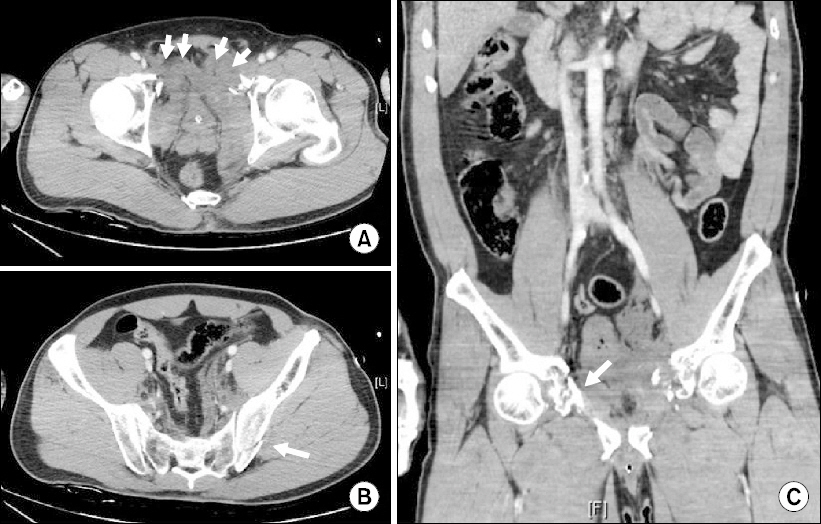
Case 1. Abdominopelvic computed tomography scan showed preperitoneal hematoma (short arrows) (A), fracture of left sacroiliac joint (white arrow) (B), and fracture of both superior and inferior rami (white arrow) (C).
A vertical skin incision of approximately 7∼8 cm was made from the symphysis pubis. After the anterior sheath of the rectus abdominis muscle was resected vertically and the muscle was split, blunt dissection was performed in a posterolateral direction to palpate the lateral border of the SI joint. Three surgical X-ray tapes were packed firmly from the near side of the SI joint (Fig. 2, 3). The same procedures were repeated on the opposite side and the skin was approximated with continuous suture. PPP was completed in only 30 minutes and then external fixation of the pelvic bone was performed by the orthopedic surgeon in 40 minutes. The right internal maxillary artery branching from the right external carotid artery was then embolized with carotid angiography to control left ear bleeding. No contrast extravasation was confirmed by pelvic angiography and the patient was transported to the trauma intensive care unit (TICU) 120 minutes after transport to OR. On the 3rd postoperative day a second operation was performed to remove surgical tapes and repair the fascia because hemodynamic instability and coagulopathy were sufficiently corrected. The patient’s mental status improved from the 10th hospital day and he finally regained consciousness. He was discharged from the TICU on the 31st hospital day. Pelvic internal fixation was not performed and the external fixator was removed on the 21st day after discharge (Table 1).

Case 1. Procedure of preperitoneal pelvic packing. (A) The patient was placed in a supine position and a vertical skin incision of approximately 7∼8 cm was made from symphysis pubis. (B) After the anterior sheath of rectus abdominis muscle was resected vertically and the muscle was split, the peritoneum was palpable with fingertips. (C) Through the preperitoneal space, blunt dissection was performed in a posterolateral direction to palpate the lateral border of the sacroiliac joint. (D) Medial migration of the peritoneum with Deaver retractor helped to improve the operation view.
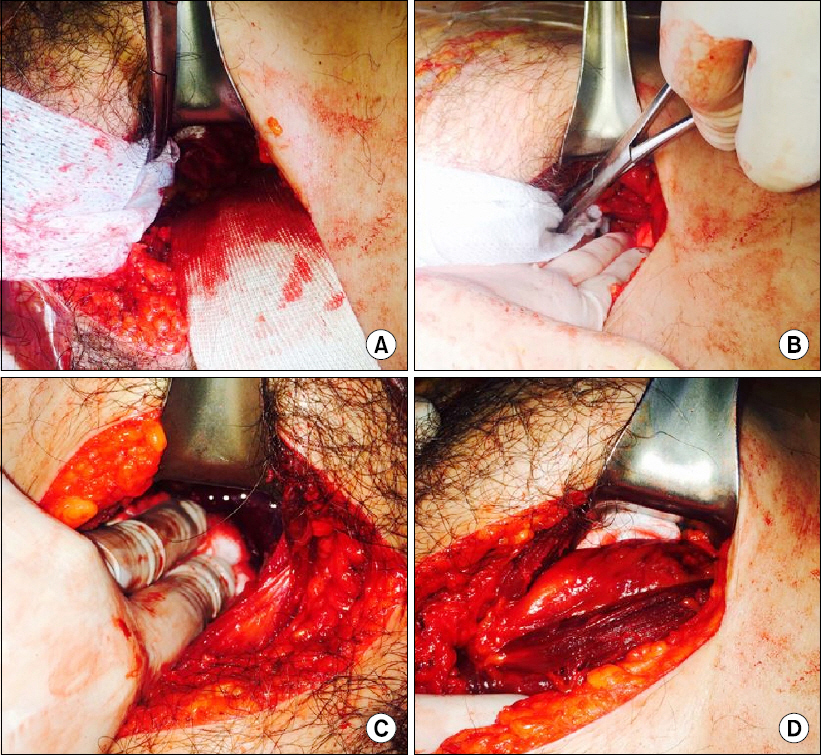
Case 1. Procedure of preperitoneal pelvic packing. (A-C) Three surgical X-ray tapes were packed firmly from the near side of the sacroiliac joint using a long Kelly clamp. (D) Packing was completed.
Case 2
A 41-year-old male truck driver presented to the trauma center with right hip pain after a car accident. In the trauma resuscitation room his blood pressure and pulse rate were 89/60 mmHg and 120/minutes, respectively. Fractures of the right iliac wing, right superior and inferior rami, and anterior acetabulum, and a large amount of hematoma in the retroperitoneum were found in APCT (Fig. 4). Base excess was -5.0 mmol/L and lactate was 4.90 mmol/L in initial ABGA. We decided to perform an emergency operation because shock persisted despite transfusion of 3 units of packed RBC. We contacted the intervention team during transport to a hybrid room in 35 minutes from admission. After completion of PPP in 35 minutes, contrast extravasation was identified in branches of the right internal iliac artery on pelvic angiography and was controlled by coil embolization (Fig. 5A, Fig. 5B). The amount of transfusion was 13 units during PPP and AE, and 4 more units of packed RBCs were transfused in the TICU over 24 hours. After the patient’s hemodynamic status and coagulopathy were improved, tape removal and internal fixation were performed on the 4th postoperative day (Fig. 5C). The patient was transferred to a general ward on the 14th hospital day (Table 1).
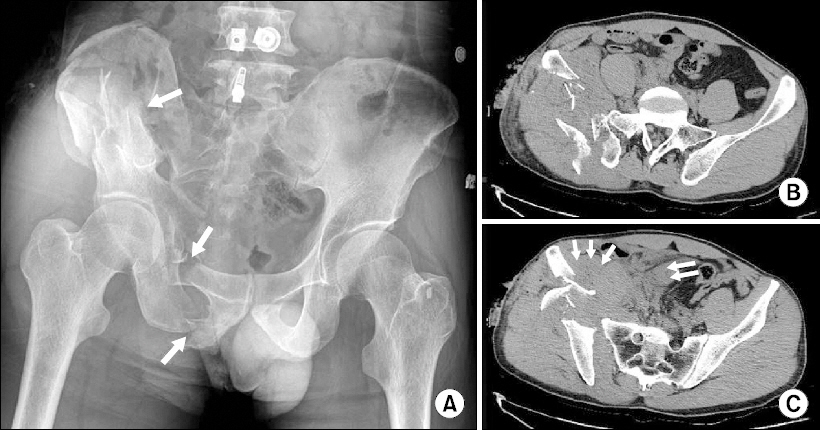
Case 2. (A) Pelvis anteroposterior X-ray showed fracture of right inferior superior rami (white arrows). Abdominopelvic computed tomography scan revealed fracture of right iliac wing (B) and massive retroperitoneal hematoma (white arrows) (C).

Case 2. (A) Pelvic angiography was performed after preperitoneal pelvic packing. (B) Hemorrhage from right internal iliac artery was controlled with coil embolization (long arrow). Packed surgical X-ray tapes were identified (short arrows). (C) Pelvis anteroposterior X-ray was taken after the second operation for tape removal and internal fixation of pelvic bone.
Discussion
Severe pelvic fracture is a life-threatening injury because it causes retroperitoneal blood loss that is difficult to control by general management. In general, the true pelvic volume is approximately 1.5 L, and 4∼6 units of RBC may be enough to tamponade pelvic hemorrhage in a stable pelvic ring. However, in cases of severe pelvic fracture with disruption of parapelvic fascia, the decreased tamponade ability will hamper hemostasis. Especially, if there is posterior displacement such as SI joint dislocation, sacral fracture, or SI joint fracture dislocation, hemorrhage from the pelvis moves into the abdominal retroperitoneal space. In this case, a blood volume of about 4∼6 L is needed to increase the pressure to 30 mmHg for tamponade formation [8]. Grimm et al.[9] demonstrated that hemorrhage escaped to retroperineum, perineum, and thigh in a cadaver model with a disrupted pelvic floor. Continuous hemorrhage causes coagulopathy and increases the bleeding tendency. In this situation, time spent on pelvic AE may be life threatening. Early PPP has several advantages in these patients. First, direct packing to the bleeding site plays a role in hemorrhage control. Second, packed surgical tapes stimulate tamponade of the pelvic cavity and lead to reduced blood loss and a decreased chance of coagulopathy. Third, PPP will block the pathway of hemorrhage migration to the abdominal retroperitoneum. Finally, the trauma surgeon can procure some time to prepare the interventional radiology team while PPP is being performed.
Because our trauma center has a hybrid OR, patients with hemodynamic instability due to pelvic fracture are transported to that room immediately and we perform PPP first. Angiography is subsequently performed in the same room if shock persists. The Denver trauma center group reported that there was no mortality due to acute hemorrhage in 75 patients with severe pelvic fracture with application of a management protocol involving PPP combined with external fixation (EF) prior to AE [7]. We have adopted this protocol, and apply PPP before AE in hemodynamically unstable patients such as the two cases presented here. Because PPP is relatively simple and can be performed in a short time, it seems to be a useful technique that can be performed with EF and AE. In the application of PPP, patient selection and timing of the procedure are important, and postoperative intensive care unit management is also essential. Appropriate resuscitation and transfusion for correction of the lethal triad (coagulopathy, metabolic acidosis, and hypothermia) are also needed, and physicians have to decide on a second operation at the point of sufficient physiologic restoration without delay. In addition, fracture of the pelvic bone has to be managed by a multidisciplinary team approach.
At the present time, PPP is not typically used in the management of pelvic fractures in Korea. These two case reports describe patients with pelvic fracture who underwent PPP after 2012, when there was a national project for the establishment of regional trauma centers. A multidisciplinary team and trauma- oriented facility are important for the management of severe pelvic fracture, and PPP can be considered as an effective method to control pelvic hemorrhage. Additional studies to determine the hemostatic effectiveness of PPP are needed.
